Vitamin D is a rising star. Vitamins A, E and beta carotene are fallen angels. And things are not looking hopeful for the rest.
The term "vitamin" comes from a contraction of the terms "vital" and "amine". Which was a concept coined by a biochemist in 1957. A not very accurate concept, because not all vitamins are "vital" , nor are they all "amines" ( a certain type of chemical that only matters to a few nerds like me. )
Which makes me somewhat embarrassed, because I have a degree in biochemistry, have been around since 1957, and yet still have no idea of whether or not vitamins are good for my patients or not ! I definitely know more about them than you do, but unfortunately that just means I am confused at a higher level !
Which makes me somewhat embarrassed, because I have a degree in biochemistry, have been around since 1957, and yet still have no idea of whether or not vitamins are good for my patients or not ! I definitely know more about them than you do, but unfortunately that just means I am confused at a higher level !
The Evils That Vitamins Do
We tend to think of vitamins as good for us, or at the very least as being natural, benign, and "essential". An attitude fostered by the thousands of companies worldwide that manufacture vitamins and try to convince people that vitamins are essential to daily living. Hence the "one a day" philosophy.
Currently Vitamin D is in fashion, for everything from stopping softening of bones to prevention of cancer. The recommended daily doses are about 1000 international units ( 1000 i.u. ) per day. But at least 10 X that much seems to be harmless, and may actually be beneficial.
Currently Vitamin D is in fashion, for everything from stopping softening of bones to prevention of cancer. The recommended daily doses are about 1000 international units ( 1000 i.u. ) per day. But at least 10 X that much seems to be harmless, and may actually be beneficial.
Vitamins may cause cancer !

We used to think that Vitamin E was good for preventing everything from heart disease to Alzheimer's. But further study, on thousands of people and at great expense, has failed to show any significant benefits. And it looks like Vit E increases the risks of prostate cancer by about 17% .
Vitamin A and it's cousin Beta Carotene were supposed to be good for everything from acne to cancer. Until further study showed that they may actually increase cancers, especially lung cancer ! Whoops !
Vitamin A and it's cousin Beta Carotene were supposed to be good for everything from acne to cancer. Until further study showed that they may actually increase cancers, especially lung cancer ! Whoops !
The wrong people are taking vitamins

The basic medical myth is that vitamins are good for you :
- this may be right for some vitamins and some people, wrong for other vitamins and other people, and irrelevant for most people and most circumstances.
- there is minimal evidence that vitamins are good for anyone, some evidence that they are bad for some people, and all sorts of evidence that the wrong people are taking vitamins.
- in an ideal world people would eat a healthy diet and get all their vitamins that natural way. From their healthy diet !
- in our medically mythical world, people who diets are less than ideal - whether due to poverty, ignorance, or alien mind control - would take vitamins to make up for their dietary deficiencies. (Man does not live by Big Macs alone !)
- the huge flaw in this philosophy is that people who are nutritionally challenged, whether due to poverty, stupidity, apathy, or alien mind control , are NOT the people who regularly take vitamins.
- the people who regularly take vitamins are neurotic yuppies with good diets, good lifestyles, good education, and enough spare cash to spend on frivolous pharmaceuticals.
- and the greatest irony is ... the vitamins may be killing off the health junkies at a rate of about 2% a year more than if they stayed at home, drank beer, and didn't take vitamins at all !
- this may be right for some vitamins and some people, wrong for other vitamins and other people, and irrelevant for most people and most circumstances.
- there is minimal evidence that vitamins are good for anyone, some evidence that they are bad for some people, and all sorts of evidence that the wrong people are taking vitamins.
- in an ideal world people would eat a healthy diet and get all their vitamins that natural way. From their healthy diet !
- in our medically mythical world, people who diets are less than ideal - whether due to poverty, ignorance, or alien mind control - would take vitamins to make up for their dietary deficiencies. (Man does not live by Big Macs alone !)
- the huge flaw in this philosophy is that people who are nutritionally challenged, whether due to poverty, stupidity, apathy, or alien mind control , are NOT the people who regularly take vitamins.
- the people who regularly take vitamins are neurotic yuppies with good diets, good lifestyles, good education, and enough spare cash to spend on frivolous pharmaceuticals.
- and the greatest irony is ... the vitamins may be killing off the health junkies at a rate of about 2% a year more than if they stayed at home, drank beer, and didn't take vitamins at all !
The secret about vitamins that doctors don't want you to know !

If you believe the above headline you already have problems. Doctors don't have any secrets. We are not organized and disciplined enough !
But the facts (as of right now ) about Vitamins are that :
1) Vitamin supplements are NOT a substitute for eating a healthy diet and leading a healthy lifestyle
2) Most vitamins don't make you healthier, and may actually increase your chances of death by about 5%
But the facts (as of right now ) about Vitamins are that :
1) Vitamin supplements are NOT a substitute for eating a healthy diet and leading a healthy lifestyle
2) Most vitamins don't make you healthier, and may actually increase your chances of death by about 5%
.

3) Even if most vitamins were actually good for us, it would be the wrong people who are taking them :
- poor folk with deficient diets are the ones who might theoretically benefit from vitamins. But they ain't the ones what takes 'em !
- it is the health conscious moneyed folk with good diets and more money than they need who drive the vitamin market. And who die slightly more.
- poor folk with deficient diets are the ones who might theoretically benefit from vitamins. But they ain't the ones what takes 'em !
- it is the health conscious moneyed folk with good diets and more money than they need who drive the vitamin market. And who die slightly more.
The question no one can answer. Yet.

Why ?
Why do voracious vitamin-munching vixens actually die sllightly more than the great unwashed hoard of humanity ?
We know exactly how much more they do die. (See below) But not the reason why. There are two likely answers :
a) Something about some vitamins is mildly deadly to health conscious yuppies.
OR
b) Health conscious yuppies are taking vitamins in the first place because they are worried about some health risk they have. And this 'hidden risk factor' is why they bite the dust at an increased rate.
The answer to this question may take years to answer. But in the meantime it is probably safest to go easy on the vitamins. You may live longer.
Why do voracious vitamin-munching vixens actually die sllightly more than the great unwashed hoard of humanity ?
We know exactly how much more they do die. (See below) But not the reason why. There are two likely answers :
a) Something about some vitamins is mildly deadly to health conscious yuppies.
OR
b) Health conscious yuppies are taking vitamins in the first place because they are worried about some health risk they have. And this 'hidden risk factor' is why they bite the dust at an increased rate.
The answer to this question may take years to answer. But in the meantime it is probably safest to go easy on the vitamins. You may live longer.
The list of deadly vitamins ( and how deadly they are ) ( to women)

- multivitamins 2.4%
- vitamin B6 4.1%
- folic acid 5.9%
- iron 3.9%
- magnesium 3.6%
- zinc 3.0%
- copper 18.0%
The Calcium Controversy
Calcium has got me really confused. Currently there are expert opinions that Calcium is both really good and really bad.
The folks who think they have proof that Calcium is deadly feel that it might be due to sudden pulses of Calcium from pills sticking on to atherosclerotic deposits in your arteries and making them hard and calcified.
Soooo....
Calcium is a mystery. But the best way to currently get Calcium into your system safely is to do it slow and gradual - with a diet rich in Calcium that leaks it slowly into your system. Which means lots of dairy products. And no Calcium pills !
The folks who think they have proof that Calcium is deadly feel that it might be due to sudden pulses of Calcium from pills sticking on to atherosclerotic deposits in your arteries and making them hard and calcified.
Soooo....
Calcium is a mystery. But the best way to currently get Calcium into your system safely is to do it slow and gradual - with a diet rich in Calcium that leaks it slowly into your system. Which means lots of dairy products. And no Calcium pills !
Vitamins can be good or bad !

Half of all U.S. adults say they take at least one dietary supplement, especially vitamins and minerals.
Pills are a huge business — $22 billion a year, by some estimates.
But none of them are subject to anything near the rigorous testing and safety requirements of prescription and over-the-counter drugs.
So manufacturers can claim benefits that aren't supported by science. They don't even have to be slightly true !
Good Vitamins

Some vitamins are almost certainly good for us.
Vitamin D, essential for healthy bones, is deficient in many people who get little sunlight and in the elderly.
Vitamin B12, important to normal brain function, often isn't well absorbed from food by older people. Childbearing women require daily folic acid supplements to reduce the risk of giving birth to children with neural tube defects.
And under medical supervision, even so-called meal replacements — high-protein, low-fat, vitamin- and mineral-rich shakes — can be a safe and effective way to lose weight and reduce the risk of obesity-related diseases.
Vitamin D, essential for healthy bones, is deficient in many people who get little sunlight and in the elderly.
Vitamin B12, important to normal brain function, often isn't well absorbed from food by older people. Childbearing women require daily folic acid supplements to reduce the risk of giving birth to children with neural tube defects.
And under medical supervision, even so-called meal replacements — high-protein, low-fat, vitamin- and mineral-rich shakes — can be a safe and effective way to lose weight and reduce the risk of obesity-related diseases.
Bad Vitamins

Excessive doses of certain vitamins and minerals are associated with increased disease risk. They fret that too many consumers equate "natural" with "safe." If nothing else, they contend, much of the billions spent on supplements is simply money wasted.
Learn more about how nutrition can help you maintain a healthy lifestyle, including natural remedies, vitamins and minerals, weight management and the impact of nutrition on aging and disease. Visit the UCLA Center for Human Nutrition.
Multivitamins/multiminerals are by far the most widely used supplements; however, among the biomedical establishment the jury is still out on their value. In 2006, an independent panel assembled by the National Institutes of Health concluded after an assessment of available evidence that more studies are needed to determine whether the popular supplements should be used to prevent major chronic illnesses such as cancer and heart disease.
And the issues are highly political.
The mainstream food and drug industry is on one side.
The organic fruit and nuts crowd is on the other side.
And both sides spew a lot of unscientific guff.
So what do you do ?
Learn more about how nutrition can help you maintain a healthy lifestyle, including natural remedies, vitamins and minerals, weight management and the impact of nutrition on aging and disease. Visit the UCLA Center for Human Nutrition.
Multivitamins/multiminerals are by far the most widely used supplements; however, among the biomedical establishment the jury is still out on their value. In 2006, an independent panel assembled by the National Institutes of Health concluded after an assessment of available evidence that more studies are needed to determine whether the popular supplements should be used to prevent major chronic illnesses such as cancer and heart disease.
And the issues are highly political.
The mainstream food and drug industry is on one side.
The organic fruit and nuts crowd is on the other side.
And both sides spew a lot of unscientific guff.
So what do you do ?
Anti-vitamins can be good !
Folks often say that doctors don't know about vitamins.
(But those same folks are often trying to sell you a herbal enema.)
This may be true of individual doctors.
Keeping up with all the latest controversies in vitaminology would be a full time job.
But medicine as a whole knows more than anyone about vitamins and supplements. Because we use them to fight disease. And sometimes fight them to cure disesase.
(But those same folks are often trying to sell you a herbal enema.)
This may be true of individual doctors.
Keeping up with all the latest controversies in vitaminology would be a full time job.
But medicine as a whole knows more than anyone about vitamins and supplements. Because we use them to fight disease. And sometimes fight them to cure disesase.
Germs and Cancers need vitamins too !

Sulpha drugs are one of the oldest and most beneficial classes of antibiotics we have.
The inhibit the use of folic acid - by bacteria.
So they kill germs by keeping them from getting at essential vitamins.
The drug "coumadin" keeps many elderly patients from having strokes. It works by interfering with production of deadly clots that go to the brain. But the body needs Vitamin K to produce those clots. By blocking production of Vitamin K
Germs need iron too. So many "iron deficient states" in patients are actually the bodies way of fighting off infections.
Even cancers need vitamins and minerals. So some of our most potent anti - cancer drugs work by depriving cancers of the nutrients that they need to grow in a wild and unrestrained fashion.
The inhibit the use of folic acid - by bacteria.
So they kill germs by keeping them from getting at essential vitamins.
The drug "coumadin" keeps many elderly patients from having strokes. It works by interfering with production of deadly clots that go to the brain. But the body needs Vitamin K to produce those clots. By blocking production of Vitamin K
Germs need iron too. So many "iron deficient states" in patients are actually the bodies way of fighting off infections.
Even cancers need vitamins and minerals. So some of our most potent anti - cancer drugs work by depriving cancers of the nutrients that they need to grow in a wild and unrestrained fashion.
The Deadly Details ...

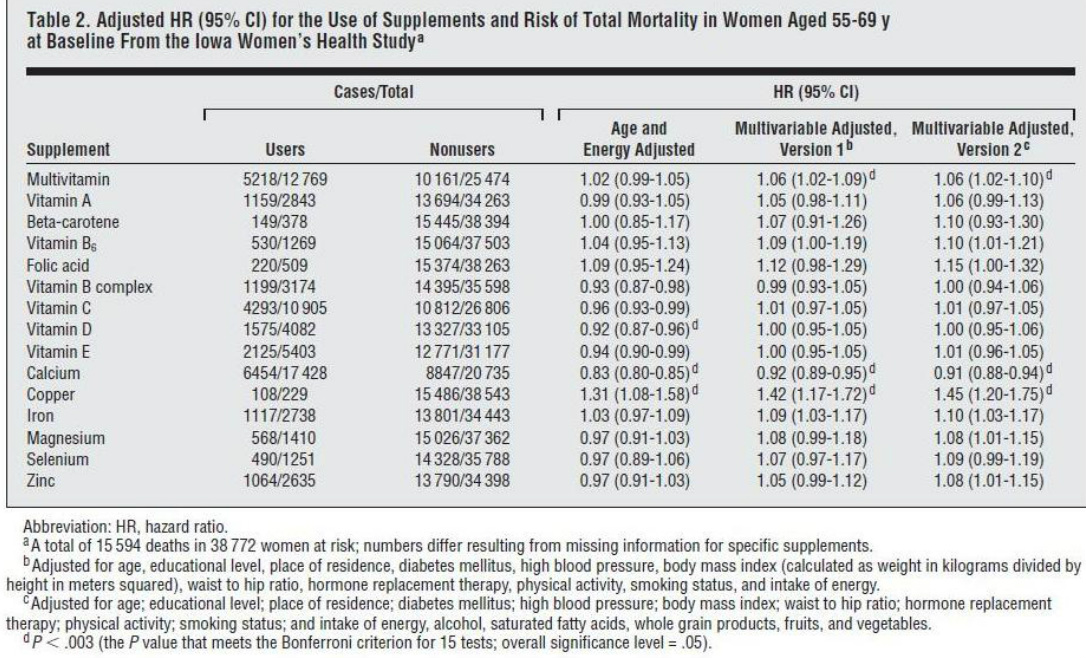
A recently published analysis of data from the Iowa Women's Health Study by Dr. Mursu and his colleagues concluded that in older women, several commonly used dietary vitamin and mineral supplements, including multivitamins, folic acid, iron, and copper, may be associated with increased total mortality risk.[1]
Previously, researchers in the same group showed that the use of dietary supplements in the United States had increased markedly between 1986 and 2004.[2] The long-term health consequences of many of these supplements remained unknown. On the basis of the previous studies, researchers hypothesized that use of dietary supplements is not associated with a reduced rate of total mortality.
In a study supported by the National Cancer Institute, the Academy of Finland, the Finnish Cultural Foundation, and the Fulbright program, Dr. Mursu and his colleagues examined the association between vitamin and mineral supplements and mortality rate among 38,772 older women (99% white, average age 61.6 years) who provided information about diet and supplement use in 1986, 1997, and 2004 via questionnaires. Self-reported supplement use increased substantially between 1986 and 2004, with 62.7% of women reporting use of at least 1 supplement daily in 1986, 75.1% in 1997, and 85.1% in 2004. Through December 31, 2008, a total of 15,594 deaths (40.2%) were identified through the State Health Registry of Iowa and the National Death Index.
Dr. Mursu’s group found that, consistent with their original hypothesis, the use of most dietary supplements was not associated with a reduced rate of total mortality. In contrast, in this multivariable-adjusted analysis, many supplements were associated with increased risk for total mortality compared with corresponding nonuse:
The researchers acknowledged that their findings did not exclude the possibility of benefits of supplements, such as improved quality of life, but they concluded that the study raised concern about their long-term safety. "Based on existing evidence, we see little justification for the general and widespread use of dietary supplements. We recommend that they be used with strong medically based cause, such as symptomatic nutrient deficiency disease," they concluded
In an invited commentary published with the study,[6] Goran Bjelakovic, MD, DMSc (University of Nis, Nis, Serbia), and Christian Gluud, MD, DMSc (Copenhagen University Hospital, Denmark), noted that its findings added to "the growing evidence demonstrating that certain antioxidant supplements, such as vitamin E, vitamin A, and beta-carotene, can be harmful," while highlighting the difference in the result with respect to calcium, "which may require further study." They also concluded that "We cannot recommend the use of vitamin and mineral supplements as a preventive measure, at least not in a well-nourished population," adding, "Those supplements do not replace or add to the benefits of eating fruits and vegetables and may cause unwanted health consequences."
Previously, researchers in the same group showed that the use of dietary supplements in the United States had increased markedly between 1986 and 2004.[2] The long-term health consequences of many of these supplements remained unknown. On the basis of the previous studies, researchers hypothesized that use of dietary supplements is not associated with a reduced rate of total mortality.
In a study supported by the National Cancer Institute, the Academy of Finland, the Finnish Cultural Foundation, and the Fulbright program, Dr. Mursu and his colleagues examined the association between vitamin and mineral supplements and mortality rate among 38,772 older women (99% white, average age 61.6 years) who provided information about diet and supplement use in 1986, 1997, and 2004 via questionnaires. Self-reported supplement use increased substantially between 1986 and 2004, with 62.7% of women reporting use of at least 1 supplement daily in 1986, 75.1% in 1997, and 85.1% in 2004. Through December 31, 2008, a total of 15,594 deaths (40.2%) were identified through the State Health Registry of Iowa and the National Death Index.
Dr. Mursu’s group found that, consistent with their original hypothesis, the use of most dietary supplements was not associated with a reduced rate of total mortality. In contrast, in this multivariable-adjusted analysis, many supplements were associated with increased risk for total mortality compared with corresponding nonuse:
- multivitamins (hazard ratio [HR], 1.06 [95% confidence interval [CI], 1.02-1.10]; absolute risk increase [ARI], 2.4%)
- vitamin B6 (HR, 1.10 [95% CI, 1.01-1.21]; ARI, 4.1%)
- folic acid (HR,1.15 [95% CI, 1.00-1.32]; ARI, 5.9%)
- iron (HR,1.10 [95% CI, 1.03-1.17]; ARI, 3.9%)
- magnesium (HR,1.08 [95% CI, 1.01-1.15]; ARI, 3.6%)
- zinc (HR,1.08 [95% CI, 1.01-1.15]; ARI, 3.0%)
- copper (HR,1.45 [95% CI, 1.20-1.75]; ARI, 18.0%)
- Of note, use of calcium was consistently inversely related to total mortality rate (HR, 0.91 [95% CI, 0.88-0.94]; absolute risk reduction, 3.8%), in contrast to the findings of previous studies.[3-5] The findings for iron and calcium were replicated in separate analyses across shorter follow-up intervals (10, 6, and 4 years) starting in 1986, 1997, and 2004; during each interval, approximately 15% of the original participants died. A dose-response relationship was seen for supplemental iron, with significantly increased risk for mortality at progressively lower doses as women aged throughout the study. There was no dose-response relationship for calcium.
The researchers acknowledged that their findings did not exclude the possibility of benefits of supplements, such as improved quality of life, but they concluded that the study raised concern about their long-term safety. "Based on existing evidence, we see little justification for the general and widespread use of dietary supplements. We recommend that they be used with strong medically based cause, such as symptomatic nutrient deficiency disease," they concluded
In an invited commentary published with the study,[6] Goran Bjelakovic, MD, DMSc (University of Nis, Nis, Serbia), and Christian Gluud, MD, DMSc (Copenhagen University Hospital, Denmark), noted that its findings added to "the growing evidence demonstrating that certain antioxidant supplements, such as vitamin E, vitamin A, and beta-carotene, can be harmful," while highlighting the difference in the result with respect to calcium, "which may require further study." They also concluded that "We cannot recommend the use of vitamin and mineral supplements as a preventive measure, at least not in a well-nourished population," adding, "Those supplements do not replace or add to the benefits of eating fruits and vegetables and may cause unwanted health consequences."
Some Vit D controversies

To [Vitamin] D or Not to D? That Is the Question
Lisa Nainggolan
Apr 29, 2013
Drug & Reference Information
COPENHAGEN, Denmark — Two leading experts in the field of vitamin D agreed to disagree yesterday here at the 2013 European Congress on Endocrinology during a lighthearted debate on the subject of whether or not everyone needs more vitamin D.
But their arguments were backed up by some serious science, and they both concurred that there are certain groups of people in whom it is necessary to ensure that vitamin-D levels are sufficient, such as pregnant women and those at risk for or with osteoporosis. And they also agreed on one way people can obtain more vitamin D: by going out in the sun for 30 minutes per day.
Where they differed, however, was that the vitamin-D proponent, Chantal Mathieu, MD, from Catholic University, Leuven, Belgium, said the list of people who need sufficient vitamin D "is so long that it really just makes more sense to give everyone small doses."
In the opposite corner, however, Mark Cooper, MD, from University Hospital, Birmingham, United Kingdom, argued that it is really only necessary to supplement specific, at-risk groups of people. "I am an investigator in randomized clinical trials of vitamin D, and I have nothing personally against [it], and I use it in my patients. But I tend to give it to people who actually need it, and that doesn't really include most of us," he observed.
And Dr. Cooper — who noted that there is a huge sector of the scientific community that is "evangelical" in its pro–vitamin-D stance — warned that physicians have been here before, with many other nutrients that subsequently, in large intervention trials, turned out to have a null effect or even be harmful. In fact, there is already evidence of risks with supplements of vitamin D from randomized clinical trials, with no evidence of benefit, he argued.
"Vitamin D — we all need more? Most of us don't, and more could actually do more harm than good."
What Does Vitamin D Do, and How Is "Deficiency" Defined?
Dr. Mathieu said the key role of vitamin D "is to promote resorption of calcium via the gut. One big lesson from all of the literature is that vitamin-D deficiency is not only bad because it's vitamin-D deficiency, but it also creates a bad calcemic status."
Vitamin-D deficiency is generally defined as a level of less than 20 ng/mL (<50 nm/L), and there are correlations in large observational studies "indicating that if you are vitamin-D deficient you get more cancer, especially colon cancer, you get more cardiovascular diseases, your immune system doesn't function properly, and overall you have a higher risk of dying," she stressed.
Going out in the sun is one option to boost vitamin D, she explained, noting that "even the dermatologists in Australia have reversed their zero-tolerance stance on the sun" in the past 2 years and conceded that 15 to 30 minutes per day in the sun "is allowed because it gives benefits." Nevertheless, the benefits must be balanced with the risks, she added, noting that "it's exactly the same wavelength of UV that you need to make vitamin D that also causes skin damage, aging, and skin cancers. So go back to nature and expose yourself to the sun, but do it with caution."
And she noted that UV rays in Northern Hemisphere winters are not strong enough to produce adequate levels of vitamin D, regardless of how long is spent in the sun. In addition, darker-skinned people, particularly those who do not expose themselves to the sun or who cover themselves, are particularly at risk. "We still see rickets in my country, in dark-skinned children who are exclusively breast-fed and whose mothers avoid the sun or are covered," she observed.
"You can also take it from foods," she explained, but added that the "only really rich food source" of vitamin D is cod-liver oil. "Salmon and mackerel from the ocean is a good source"; however, most of this fish is now bred in farms, and farm-bred fish do not have a lot of vitamin D.
If our skin cannot make enough vitamin D under the UV, just give vitamin D, give the hormone.Dr. Chantal Mathieu
"So what do we do? We are endocrinologists. If the thyroid fails, we give thyroid-hormone substitution. If our skin cannot make enough vitamin D under the UV, just give vitamin D, give the hormone itself."
But the key, she said, is to use smaller doses of vitamin D than have previously been recommended. The US Endocrine Society guidance, for example, advises supplementation with up to 2000 IU per day, but this is overzealous, she said. "A more reasonable dose is 600 to 800 IU per day," she noted, adding that she is an author on a new guidance, soon to be published in the Journal of Clinical Endocrinology and Metabolism, which will state that 2000 IU per day "is not warranted."
"So my conclusion, yes, we all need more vitamin D, but we don't need crazy high doses."
In response, Dr. Cooper conceded: "Our natural state of vitamin D is much higher than we have today — we live indoors too much — and lower levels of vitamin D have been linked with cancer, heart disease, increases in diabetes, shortened life, the list goes on, and it's a very long list. In fact, you will do well to find a condition that isn't linked with too little vitamin D." But the problem, said Dr. Cooper, is that "the supposed benefits of vitamin D are exclusively reported in observational studies. We really need some robust evidence."
Vitamin-D Intervention Trials to Date "Mostly Negative"
Dr. Mathieu, Dr. Cooper said, had alluded to randomized trials in the future, "but we have got lots of randomized trials now," he argued, quoting a "typical" one, the RECORD trial from the United Kingdom.
This looked at vitamin-D supplementation and fractures in 5000 community-dwelling women and wasreported in the Lancet in 2005. "What it showed was that if you took vitamin D from [a level of] 38 nm/L, the average in that population on placebo, and raised it to 62 nm/L, which is a very useful increase — what does it do? Absolutely nothing, [at least] to falls and fractures."
And there have been "lots" of other randomized controlled trials, he added, "and my view is that these are mostly negative. The Women's Health Initiative, with 36,000 people [taking vitamin D] combined with calcium, didn't show any effect whatsoever. It did show, however, that [vitamin D plus calcium] caused kidney stones, a 70% increase, which is not medically insignificant."
Vitamin D holds the record for the most number of meta-analyses for the fewest number of trials.Dr. Mark Cooper
He noted also that in the attempts to find some benefit, "Vitamin D holds the record for the most number of meta-analyses for the fewest number of trials," and the results generally "depend on who does the meta-analysis. Those who do not have a major ax to grind (eg, the Institute of Medicine [IOM]), tend to come up with negative results, whereas those who really believe in vitamin D seem to get positive results with their meta-analysis."
And then there are those who say "maybe we are not getting levels high enough, we need to get over a certain threshold of intake," he observed. "But there have been trials in recent years that have done this, too."
He cited one from JAMA (2010;303:1815-1822), performed in Australia in the winter in women, giving them very high doses. The women in the active-treatment group ended up with levels of vitamin D of 75 nm/L, "so it worked" in comparison with the placebo group, who had average levels of 50 nm/L. "But the result was vitamin D caused a significant excess of falls and fractures. One in 3 people had an extra fall due to the vitamin D. This is not good."
He then went on to discuss the editorial accompanying this study, "which gave the explanation that the reason falls increased was because vitamin D was too good, the people who got it felt so well, they came to harm because they were having such increased functional mobility. Clearly ridiculous, but it gives you a mind-set of how people think about vitamin D."
He went on to list a number of other, recent randomized clinical trials with vitamin D, for conditions such as cognition, muscle strength, cancer, osteoarthritis, TB, etc. "Different doses of vitamin D, different groups, all well-designed, all in major journals, and all negative." He added that at least 1 in 20 of these studies "should be positive" just by chance, "but we haven't seen that yet."
Does a Little Suboptimal Absorption of Calcium Matter?
In rebuttal, however, Dr. Matheiu said all of the intervention studies "struggle with compliance issues, we all know that if we need to take a pill every day for 1 year, we will start to forget. So all the intervention studies you have seen give vitamin D in megadoses once every month, once every 2 months. That's not what I mean as 'we all need more.'
"Where we are now is a mean of 20 to 25 ng/mL, so if we want to analyze this objectively, half of our population is deficient. We all need more vitamin D than we are getting now. Saudi Arabia has a mean level of vitamin D that is below 20 ng/mL; should we wait to supplement people in Saudi? We know they are all vitamin-D deficient because it's too hot to get out in the sun.
Where we are now is a mean of 20 to 25 ng/mL; half of our population is deficient.Dr. Chantal Mathieu
"Vitamin-D deficiency in all of our association studies is clearly associated with impaired outcomes. We know that restoration of vitamin-D deficiency with small doses avoids adverse outcomes. I do not think we can afford to sit and wait for well-designed intervention studies," she stressed.
And, she argues, "It's too expensive to go around and measure vitamin-D levels in everybody. My argument would be to stop measuring levels in everybody. It's nonsense. There is a very easy way to prevent all of this, and that is to give small doses of vitamin D to the whole population, and that's what the IOM says. They say in children below 1 year of age, 400 IU per day; in individuals older than 70 years of age, 800 IU per day; and all of the rest, all of us, 600 IU of vitamin D every day. So yes! We all need more."
She did concede, however, that here are a few potential exceptions, such as patients with kidney stones "in whom you need to be careful."
In his rebuttal, Dr. Cooper replied, "Clearly, we agree on many things. Those populations at risk of rickets or hypocalcemia need vitamin D. Pregnancy is a situation where, clearly, you want to make sure levels are adequate" — although he acknowledged there has recently been debate on this issue — "and having vitamin D in the treatment of osteoporosis is mandatory, because you don't want to risk someone having even a small deficiency. But for the rest of the population, what does a little bit of suboptimal absorption of calcium matter? Who cares?
All of the primary analyses of the intervention studies described previously bear out the fact that there is no evidence of any benefit with vitamin D for the most part, he stressed.
"You can get on-the-spot tests for vitamin D now. And we are doing loads of vitamin-D assays. We are making everybody anxious. We [endocrinologists] ourselves are anxious. We shouldn't worry everybody, we should have good, balanced nutrition, but the majority of people who are otherwise healthy and asymptomatic shouldn't go around taking supplements.
"Will having a higher vitamin-D level give you a healthier, longer life? You can't do a randomized trial for 50 or 60 years, which is what you need to address this. More work needs to be done, clearly, but it's a tricky area," he concluded.
Drs. Mathieu and Cooper have reported no relevant financial relationships.
2013 European Congress of Endocrinology. Debate 1, presented April 28, 2013.
Lisa Nainggolan
Apr 29, 2013
- Pregnancy Vitamin-D Levels Do Not Affect Bones of Kids
- Endocrine Society Issues Practice Guideline on Vitamin D
Drug & Reference Information
COPENHAGEN, Denmark — Two leading experts in the field of vitamin D agreed to disagree yesterday here at the 2013 European Congress on Endocrinology during a lighthearted debate on the subject of whether or not everyone needs more vitamin D.
But their arguments were backed up by some serious science, and they both concurred that there are certain groups of people in whom it is necessary to ensure that vitamin-D levels are sufficient, such as pregnant women and those at risk for or with osteoporosis. And they also agreed on one way people can obtain more vitamin D: by going out in the sun for 30 minutes per day.
Where they differed, however, was that the vitamin-D proponent, Chantal Mathieu, MD, from Catholic University, Leuven, Belgium, said the list of people who need sufficient vitamin D "is so long that it really just makes more sense to give everyone small doses."
In the opposite corner, however, Mark Cooper, MD, from University Hospital, Birmingham, United Kingdom, argued that it is really only necessary to supplement specific, at-risk groups of people. "I am an investigator in randomized clinical trials of vitamin D, and I have nothing personally against [it], and I use it in my patients. But I tend to give it to people who actually need it, and that doesn't really include most of us," he observed.
And Dr. Cooper — who noted that there is a huge sector of the scientific community that is "evangelical" in its pro–vitamin-D stance — warned that physicians have been here before, with many other nutrients that subsequently, in large intervention trials, turned out to have a null effect or even be harmful. In fact, there is already evidence of risks with supplements of vitamin D from randomized clinical trials, with no evidence of benefit, he argued.
"Vitamin D — we all need more? Most of us don't, and more could actually do more harm than good."
What Does Vitamin D Do, and How Is "Deficiency" Defined?
Dr. Mathieu said the key role of vitamin D "is to promote resorption of calcium via the gut. One big lesson from all of the literature is that vitamin-D deficiency is not only bad because it's vitamin-D deficiency, but it also creates a bad calcemic status."
Vitamin-D deficiency is generally defined as a level of less than 20 ng/mL (<50 nm/L), and there are correlations in large observational studies "indicating that if you are vitamin-D deficient you get more cancer, especially colon cancer, you get more cardiovascular diseases, your immune system doesn't function properly, and overall you have a higher risk of dying," she stressed.
Going out in the sun is one option to boost vitamin D, she explained, noting that "even the dermatologists in Australia have reversed their zero-tolerance stance on the sun" in the past 2 years and conceded that 15 to 30 minutes per day in the sun "is allowed because it gives benefits." Nevertheless, the benefits must be balanced with the risks, she added, noting that "it's exactly the same wavelength of UV that you need to make vitamin D that also causes skin damage, aging, and skin cancers. So go back to nature and expose yourself to the sun, but do it with caution."
And she noted that UV rays in Northern Hemisphere winters are not strong enough to produce adequate levels of vitamin D, regardless of how long is spent in the sun. In addition, darker-skinned people, particularly those who do not expose themselves to the sun or who cover themselves, are particularly at risk. "We still see rickets in my country, in dark-skinned children who are exclusively breast-fed and whose mothers avoid the sun or are covered," she observed.
"You can also take it from foods," she explained, but added that the "only really rich food source" of vitamin D is cod-liver oil. "Salmon and mackerel from the ocean is a good source"; however, most of this fish is now bred in farms, and farm-bred fish do not have a lot of vitamin D.
If our skin cannot make enough vitamin D under the UV, just give vitamin D, give the hormone.Dr. Chantal Mathieu
"So what do we do? We are endocrinologists. If the thyroid fails, we give thyroid-hormone substitution. If our skin cannot make enough vitamin D under the UV, just give vitamin D, give the hormone itself."
But the key, she said, is to use smaller doses of vitamin D than have previously been recommended. The US Endocrine Society guidance, for example, advises supplementation with up to 2000 IU per day, but this is overzealous, she said. "A more reasonable dose is 600 to 800 IU per day," she noted, adding that she is an author on a new guidance, soon to be published in the Journal of Clinical Endocrinology and Metabolism, which will state that 2000 IU per day "is not warranted."
"So my conclusion, yes, we all need more vitamin D, but we don't need crazy high doses."
In response, Dr. Cooper conceded: "Our natural state of vitamin D is much higher than we have today — we live indoors too much — and lower levels of vitamin D have been linked with cancer, heart disease, increases in diabetes, shortened life, the list goes on, and it's a very long list. In fact, you will do well to find a condition that isn't linked with too little vitamin D." But the problem, said Dr. Cooper, is that "the supposed benefits of vitamin D are exclusively reported in observational studies. We really need some robust evidence."
Vitamin-D Intervention Trials to Date "Mostly Negative"
Dr. Mathieu, Dr. Cooper said, had alluded to randomized trials in the future, "but we have got lots of randomized trials now," he argued, quoting a "typical" one, the RECORD trial from the United Kingdom.
This looked at vitamin-D supplementation and fractures in 5000 community-dwelling women and wasreported in the Lancet in 2005. "What it showed was that if you took vitamin D from [a level of] 38 nm/L, the average in that population on placebo, and raised it to 62 nm/L, which is a very useful increase — what does it do? Absolutely nothing, [at least] to falls and fractures."
And there have been "lots" of other randomized controlled trials, he added, "and my view is that these are mostly negative. The Women's Health Initiative, with 36,000 people [taking vitamin D] combined with calcium, didn't show any effect whatsoever. It did show, however, that [vitamin D plus calcium] caused kidney stones, a 70% increase, which is not medically insignificant."
Vitamin D holds the record for the most number of meta-analyses for the fewest number of trials.Dr. Mark Cooper
He noted also that in the attempts to find some benefit, "Vitamin D holds the record for the most number of meta-analyses for the fewest number of trials," and the results generally "depend on who does the meta-analysis. Those who do not have a major ax to grind (eg, the Institute of Medicine [IOM]), tend to come up with negative results, whereas those who really believe in vitamin D seem to get positive results with their meta-analysis."
And then there are those who say "maybe we are not getting levels high enough, we need to get over a certain threshold of intake," he observed. "But there have been trials in recent years that have done this, too."
He cited one from JAMA (2010;303:1815-1822), performed in Australia in the winter in women, giving them very high doses. The women in the active-treatment group ended up with levels of vitamin D of 75 nm/L, "so it worked" in comparison with the placebo group, who had average levels of 50 nm/L. "But the result was vitamin D caused a significant excess of falls and fractures. One in 3 people had an extra fall due to the vitamin D. This is not good."
He then went on to discuss the editorial accompanying this study, "which gave the explanation that the reason falls increased was because vitamin D was too good, the people who got it felt so well, they came to harm because they were having such increased functional mobility. Clearly ridiculous, but it gives you a mind-set of how people think about vitamin D."
He went on to list a number of other, recent randomized clinical trials with vitamin D, for conditions such as cognition, muscle strength, cancer, osteoarthritis, TB, etc. "Different doses of vitamin D, different groups, all well-designed, all in major journals, and all negative." He added that at least 1 in 20 of these studies "should be positive" just by chance, "but we haven't seen that yet."
Does a Little Suboptimal Absorption of Calcium Matter?
In rebuttal, however, Dr. Matheiu said all of the intervention studies "struggle with compliance issues, we all know that if we need to take a pill every day for 1 year, we will start to forget. So all the intervention studies you have seen give vitamin D in megadoses once every month, once every 2 months. That's not what I mean as 'we all need more.'
"Where we are now is a mean of 20 to 25 ng/mL, so if we want to analyze this objectively, half of our population is deficient. We all need more vitamin D than we are getting now. Saudi Arabia has a mean level of vitamin D that is below 20 ng/mL; should we wait to supplement people in Saudi? We know they are all vitamin-D deficient because it's too hot to get out in the sun.
Where we are now is a mean of 20 to 25 ng/mL; half of our population is deficient.Dr. Chantal Mathieu
"Vitamin-D deficiency in all of our association studies is clearly associated with impaired outcomes. We know that restoration of vitamin-D deficiency with small doses avoids adverse outcomes. I do not think we can afford to sit and wait for well-designed intervention studies," she stressed.
And, she argues, "It's too expensive to go around and measure vitamin-D levels in everybody. My argument would be to stop measuring levels in everybody. It's nonsense. There is a very easy way to prevent all of this, and that is to give small doses of vitamin D to the whole population, and that's what the IOM says. They say in children below 1 year of age, 400 IU per day; in individuals older than 70 years of age, 800 IU per day; and all of the rest, all of us, 600 IU of vitamin D every day. So yes! We all need more."
She did concede, however, that here are a few potential exceptions, such as patients with kidney stones "in whom you need to be careful."
In his rebuttal, Dr. Cooper replied, "Clearly, we agree on many things. Those populations at risk of rickets or hypocalcemia need vitamin D. Pregnancy is a situation where, clearly, you want to make sure levels are adequate" — although he acknowledged there has recently been debate on this issue — "and having vitamin D in the treatment of osteoporosis is mandatory, because you don't want to risk someone having even a small deficiency. But for the rest of the population, what does a little bit of suboptimal absorption of calcium matter? Who cares?
All of the primary analyses of the intervention studies described previously bear out the fact that there is no evidence of any benefit with vitamin D for the most part, he stressed.
"You can get on-the-spot tests for vitamin D now. And we are doing loads of vitamin-D assays. We are making everybody anxious. We [endocrinologists] ourselves are anxious. We shouldn't worry everybody, we should have good, balanced nutrition, but the majority of people who are otherwise healthy and asymptomatic shouldn't go around taking supplements.
"Will having a higher vitamin-D level give you a healthier, longer life? You can't do a randomized trial for 50 or 60 years, which is what you need to address this. More work needs to be done, clearly, but it's a tricky area," he concluded.
Drs. Mathieu and Cooper have reported no relevant financial relationships.
2013 European Congress of Endocrinology. Debate 1, presented April 28, 2013.