Patello - Femoral Pain Syndrome (Chondromalacia patella)
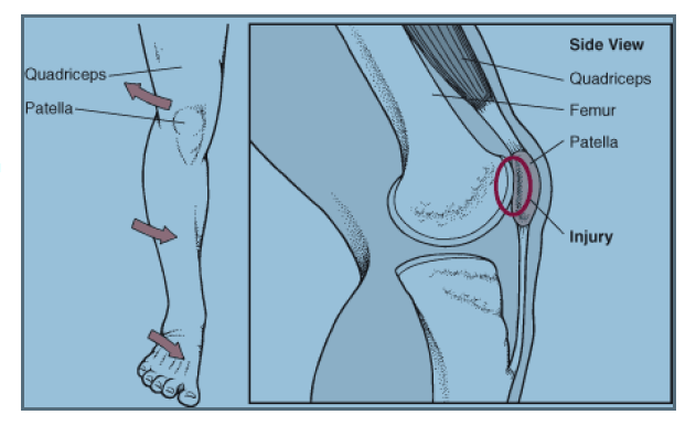
Click on the diagram above to lead to a site that gives a good description of the basics.
Click here to see patellofemoral pain, "the movie" ( no academy awards, but a good explanation and a cute accent )
And in other words ...
Patellofemoral pain syndrome (PFPS) is a syndrome characterized by pain or discomfort seemingly originating from the contact of the posterior surface of the patella (back of the kneecap) with the femur (thigh bone). It is the most frequently encountered diagnosis in sports medicine clinics.
The cause of pain and dysfunction often results from either abnormal forces (e.g. increased pull of the lateral quadricep retinaculum with acute or chronic lateral PF subluxation/dislocation) or prolonged repetitive compressive or shearing forces (running or jumping) on the PF joint. The result is thinning and softening (chondromalacia) of the articular cartilage under the patella and/or on the medial or lateral femoral condyles, synovial irritation and inflammation and subchondral bony changes in the distal femur or patella known as "bone bruises". Secondary causes of PF Syndrome are fractures, internal knee derangement, OA of the knee and bony tumors in or around the knee.[1]
Specific populations at high risk of primary Patellofemoral Syndrome include runners, bicyclists, basketball players, young athletes and females especially those who have an increased angle of genu valgus (aka "Q-Angle" or commonly referred to as "knock-knees"). Typically patients will complain of localized anterior knee pain which is exacerbated by sports, walking, sitting for a long time, or stair climbing. Descending stairs may be worse than ascending. Unless there is an underlying pathology in the knee, swelling is usually mild to nil. Palpation, as well, is usually unremarkable.
Treatment
Exercises
Quadriceps strengthening is commonly suggested because the quadricep muscles help to stabilize the patella. Proper form is very important. Inflexibility has often been cited as a source of patellofemoral pain syndrome. Stretching of the hip, hamstring, calf (anatomy), and iliotibial band may help restore proper biomechanics. Furthermore, the use of a foam roller may help to add flexibility and relieve pain from sore or stiff muscles in the leg.
Rest
Patellofemoral pain syndrome may also result from overuse or overload of the PF joint. For this reason, knee activity should be reduced until the pain is resolved.[4][5] Those with pain originating from sitting too long should straighten the leg or walk periodically. Those who engage in high impact activity such as running should consider a nonimpact activity such as swimming or aerobics on an elliptical machine.
Ice and medication
To reduce inflammation, ice can be applied to the PF joint after an activity. The ice should be kept in place for 10 to 15 minutes. Additionally anti-inflammatory drugs such NSAIDs can also be taken immediately after an activity.
Orthosis and taping:
In addition to physical therapy, external devices such as patellofemoral knee orthosis and tape could be used to stabilize the knee. These orthoses will not correct the underlying source but may prevent further injury. For this reason, they should be used in conjunction with and not in lieu of physical therapy. The technique of McConnell taping has been helpful in some studies.
Arch support
Low arches can cause overpronation or the feet to roll inward too much increasing the Q angle and genu valgus. Poor lower extremity biomechanics may cause stress on the knees and ultimately patellofemoral pain syndrome. Stability or motion control shoes are designed for people with pronation issues. Arch supports and custom orthotics may also help to improve lower extremity biomechanics.
The cause of pain and dysfunction often results from either abnormal forces (e.g. increased pull of the lateral quadricep retinaculum with acute or chronic lateral PF subluxation/dislocation) or prolonged repetitive compressive or shearing forces (running or jumping) on the PF joint. The result is thinning and softening (chondromalacia) of the articular cartilage under the patella and/or on the medial or lateral femoral condyles, synovial irritation and inflammation and subchondral bony changes in the distal femur or patella known as "bone bruises". Secondary causes of PF Syndrome are fractures, internal knee derangement, OA of the knee and bony tumors in or around the knee.[1]
Specific populations at high risk of primary Patellofemoral Syndrome include runners, bicyclists, basketball players, young athletes and females especially those who have an increased angle of genu valgus (aka "Q-Angle" or commonly referred to as "knock-knees"). Typically patients will complain of localized anterior knee pain which is exacerbated by sports, walking, sitting for a long time, or stair climbing. Descending stairs may be worse than ascending. Unless there is an underlying pathology in the knee, swelling is usually mild to nil. Palpation, as well, is usually unremarkable.
Treatment
Exercises
Quadriceps strengthening is commonly suggested because the quadricep muscles help to stabilize the patella. Proper form is very important. Inflexibility has often been cited as a source of patellofemoral pain syndrome. Stretching of the hip, hamstring, calf (anatomy), and iliotibial band may help restore proper biomechanics. Furthermore, the use of a foam roller may help to add flexibility and relieve pain from sore or stiff muscles in the leg.
Rest
Patellofemoral pain syndrome may also result from overuse or overload of the PF joint. For this reason, knee activity should be reduced until the pain is resolved.[4][5] Those with pain originating from sitting too long should straighten the leg or walk periodically. Those who engage in high impact activity such as running should consider a nonimpact activity such as swimming or aerobics on an elliptical machine.
Ice and medication
To reduce inflammation, ice can be applied to the PF joint after an activity. The ice should be kept in place for 10 to 15 minutes. Additionally anti-inflammatory drugs such NSAIDs can also be taken immediately after an activity.
Orthosis and taping:
In addition to physical therapy, external devices such as patellofemoral knee orthosis and tape could be used to stabilize the knee. These orthoses will not correct the underlying source but may prevent further injury. For this reason, they should be used in conjunction with and not in lieu of physical therapy. The technique of McConnell taping has been helpful in some studies.
Arch support
Low arches can cause overpronation or the feet to roll inward too much increasing the Q angle and genu valgus. Poor lower extremity biomechanics may cause stress on the knees and ultimately patellofemoral pain syndrome. Stability or motion control shoes are designed for people with pronation issues. Arch supports and custom orthotics may also help to improve lower extremity biomechanics.