Chocolate can be used to treat heart failure
Below is an article that I get a real kick out of, because it is a double blind randomized placebo controled trial to test out a drug for heart failure - chocolate.
When subjected to exactly the same scrutiny as a new cardiac drug, chocolate proved it's worth conclusively. So I know have perfect scientific and statistical justification for prescribing chocolate for all of my patients. Probably any chocolate will do, although to be strictly adherent to the terms of this study one should probably go with the chocolate used in this study. The chocolate proven to be hearth healthy was " Nestle's Noir Elite".
When subjected to exactly the same scrutiny as a new cardiac drug, chocolate proved it's worth conclusively. So I know have perfect scientific and statistical justification for prescribing chocolate for all of my patients. Probably any chocolate will do, although to be strictly adherent to the terms of this study one should probably go with the chocolate used in this study. The chocolate proven to be hearth healthy was " Nestle's Noir Elite".
Cardiovascular Effects of Flavanol-Rich Chocolate in Patients With Heart Failure
Aims
Flavanol-rich chocolate (FRC) is beneficial for vascular and platelet function by increasing nitric oxide bioavailability and decreasing oxidative stress. Congestive heart failure (CHF) is characterized by impaired endothelial and increased platelet reactivity. As statins are ineffective in CHF, alternative therapies are a clinical need. We therefore investigated whether FRC might improve cardiovascular function in patients with CHF.
Methods and results
Twenty patients with CHF were enrolled in a double-blind, randomized placebo-controlled trial, comparing the effect of commercially available FRC with cocoa-liquor-free control chocolate (CC) on endothelial and platelet function in the short term (2 h after ingestion of a chocolate bar) and long term (4 weeks, two chocolate bars/day). Endothelial function was assessed non-invasively by flow-mediated vasodilatation of the brachial artery. Flow-mediated vasodilatation significantly improved from 4.98 ± 1.95 to 5.98 ± 2.32% (P = 0.045 and 0.02 for between-group changes) 2h after intake of FRC to 6.86 ± 1.76% after 4 weeks of daily intake (P = 0.03 and 0.004 for between groups). No effect on endothelial-independent vasodilatation was observed. Platelet adhesion significantly decreased from 3.9 ± 1.3 to 3.0 ± 1.3% (P = 0.03 and 0.05 for between groups) 2 h after FRC, an effect that was not sustained at 2 and 4 weeks. Cocoa-liquor-free CC had no effect, either on endothelial function or on platelet function. Blood pressure and heart rate did not change in either group.
Conclusion
Flavanol-rich chocolate acutely improves vascular function in patients with CHF. A sustained effect was seen after daily consumption over a 4-week period, even after 12 h abstinence. These beneficial effects were paralleled by an inhibition of platelet function in the presence of FRC only.
Trial Registration ClinicalTrials.gov Identifier: NCT00538941
Flavanol-rich chocolate (FRC) is beneficial for vascular and platelet function by increasing nitric oxide bioavailability and decreasing oxidative stress. Congestive heart failure (CHF) is characterized by impaired endothelial and increased platelet reactivity. As statins are ineffective in CHF, alternative therapies are a clinical need. We therefore investigated whether FRC might improve cardiovascular function in patients with CHF.
Methods and results
Twenty patients with CHF were enrolled in a double-blind, randomized placebo-controlled trial, comparing the effect of commercially available FRC with cocoa-liquor-free control chocolate (CC) on endothelial and platelet function in the short term (2 h after ingestion of a chocolate bar) and long term (4 weeks, two chocolate bars/day). Endothelial function was assessed non-invasively by flow-mediated vasodilatation of the brachial artery. Flow-mediated vasodilatation significantly improved from 4.98 ± 1.95 to 5.98 ± 2.32% (P = 0.045 and 0.02 for between-group changes) 2h after intake of FRC to 6.86 ± 1.76% after 4 weeks of daily intake (P = 0.03 and 0.004 for between groups). No effect on endothelial-independent vasodilatation was observed. Platelet adhesion significantly decreased from 3.9 ± 1.3 to 3.0 ± 1.3% (P = 0.03 and 0.05 for between groups) 2 h after FRC, an effect that was not sustained at 2 and 4 weeks. Cocoa-liquor-free CC had no effect, either on endothelial function or on platelet function. Blood pressure and heart rate did not change in either group.
Conclusion
Flavanol-rich chocolate acutely improves vascular function in patients with CHF. A sustained effect was seen after daily consumption over a 4-week period, even after 12 h abstinence. These beneficial effects were paralleled by an inhibition of platelet function in the presence of FRC only.
Trial Registration ClinicalTrials.gov Identifier: NCT00538941
And what that means in plain English is ....
Introduction
Cocoa consumption exerts several beneficial effects on cardiovascular health.[1] Epidemiologically, its consumption is inversely correlated with blood pressure (BP) and all-cause mortality,[2] which has been recently confirmed in a large population-based study.[3] However, there are no large-scale prospective morbidity and mortality trials evaluating the effect of cocoa so far, but smaller randomized studies convincingly proved beneficial short-term effects on cardiovascular surrogates, namely on endothelial function.[1] Endothelial dysfunction is a pathophysiological condition, associated with premature atherothrombotic disease.[4] Diminished NO bioavailability and increased oxidative stress are among the most important features of endothelial dysfunction.[5] Endothelial function can be assessed non-invasively by ultrasound-guided measuring of flow-mediated dilatation (FMD) of the brachial artery. It correlates with coronary endothelial function and is predictive of future coronary events.[6–8]
Congestive heart failure (CHF) is a prevalent condition, representing the final stage of most cardiovascular diseases and is associated with high morbidity and mortality.[9] Patients with CHF typically show endothelial dysfunction, increased oxidative stress, and baroreceptor dysfunction.[10]Moreover, patients with impaired FMD are at increased risk for cardiovascular events and death[10]complications of atherosclerosis that involve increased platelet activation. Indeed, many complications in HF are thrombus-related and increased platelet activation has been observed in CHF.[11]
Cocoa acutely improve NO-dependent vasodilatation in healthy humans[12] and in patients with cardiovascular risk factors, including diabetes, both in the forearm circulation[13–15] and in coronary arteries.[16] Congestive heart failure is a very late stage of most forms of cardiovascular disease. At that stage, many cardiovascular alterations are irreversible. For instance, lowering of low-density lipoproteins by HMG coenzyme reductase inhibitors does not longer reduce the event rates even in patients with ischaemic cardiomyopathy.[17,18] Thus, alternative treatment options have to be explored in these high-risk patients. Due to its potential to enhance NO bioavailability and its antioxidative properties, flavanol-rich chocolate (FRC) might be beneficial in CHF patients. It was thus the aim of this double-blind, placebo-controlled study to evaluate both the acute (2 h after ingestion) and the longer-term (at 2 and 4 weeks) effects of FRC when compared with a cocoa-liquor-free control chocolate (CC) on endothelial and platelet function in patients with CHF.
Cocoa consumption exerts several beneficial effects on cardiovascular health.[1] Epidemiologically, its consumption is inversely correlated with blood pressure (BP) and all-cause mortality,[2] which has been recently confirmed in a large population-based study.[3] However, there are no large-scale prospective morbidity and mortality trials evaluating the effect of cocoa so far, but smaller randomized studies convincingly proved beneficial short-term effects on cardiovascular surrogates, namely on endothelial function.[1] Endothelial dysfunction is a pathophysiological condition, associated with premature atherothrombotic disease.[4] Diminished NO bioavailability and increased oxidative stress are among the most important features of endothelial dysfunction.[5] Endothelial function can be assessed non-invasively by ultrasound-guided measuring of flow-mediated dilatation (FMD) of the brachial artery. It correlates with coronary endothelial function and is predictive of future coronary events.[6–8]
Congestive heart failure (CHF) is a prevalent condition, representing the final stage of most cardiovascular diseases and is associated with high morbidity and mortality.[9] Patients with CHF typically show endothelial dysfunction, increased oxidative stress, and baroreceptor dysfunction.[10]Moreover, patients with impaired FMD are at increased risk for cardiovascular events and death[10]complications of atherosclerosis that involve increased platelet activation. Indeed, many complications in HF are thrombus-related and increased platelet activation has been observed in CHF.[11]
Cocoa acutely improve NO-dependent vasodilatation in healthy humans[12] and in patients with cardiovascular risk factors, including diabetes, both in the forearm circulation[13–15] and in coronary arteries.[16] Congestive heart failure is a very late stage of most forms of cardiovascular disease. At that stage, many cardiovascular alterations are irreversible. For instance, lowering of low-density lipoproteins by HMG coenzyme reductase inhibitors does not longer reduce the event rates even in patients with ischaemic cardiomyopathy.[17,18] Thus, alternative treatment options have to be explored in these high-risk patients. Due to its potential to enhance NO bioavailability and its antioxidative properties, flavanol-rich chocolate (FRC) might be beneficial in CHF patients. It was thus the aim of this double-blind, placebo-controlled study to evaluate both the acute (2 h after ingestion) and the longer-term (at 2 and 4 weeks) effects of FRC when compared with a cocoa-liquor-free control chocolate (CC) on endothelial and platelet function in patients with CHF.
.
Methods
Subjects
Twenty-two patients with stable CHF (NYHA ≥ II) and ejection fraction <50% have been randomized. Exclusion criteria were: decompensated HF, unstable angina pectoris, smoking, creatinine >200 µmol/L, alanine aminotransferase or aspartate aminotransferase >150 IU, diabetes mellitus, obesity (body mass index >30 kg/m2), symptomatic hypotension, BP > 160/100 mmHg, known allergies to compounds of study chocolate or placebo, respectively, history of gastric ulcer or bleeding, venous thrombosis or pulmonary embolism, history of infectious disease or systemic inflammatory diseases, malignant tumours (unless cured or in remission for more than 5 years), concomitant vitamin supplements, as well as participation in another study within the last month. Two patients dropped out during follow-up (one patient withdrew consent because of personal reasons and one patient was excluded due to ventricular fibrillation, terminated by an internal defibrillator; this event was considered unrelated to the study protocol). Twenty patients were included into the final analysis.
Flavanol-rich and CC were prepared by Nestlé. Both were wrapped identically and randomization was done by an organization independent of the study group (InterCorNet, Zürich, Switzerland).
All patients gave signed informed consent. The study was performed at the University Hospital of Zurich, and the study protocol approved by the local Ethics Committee and conducted according to the Declaration of Helsinki. Patients were recruited from the HF outpatient clinic.
Experimental Protocol
All patients were instructed to refrain from flavanol-rich food for 24 h and fast for at least 8 h before baseline examinations, which were always performed in the morning. After a short clinical examination and blood sampling, baseline measurements were performed. Blood pressure was measured three times with a validated automatic BP device (OMRON Mit Elite Plus). The mean of the last two measurements was recorded. Following the first assessment, the participants were randomized to receive either 40 g of FRC or 28.4 g of CC (weight matched for fat and sugar content to the dark chocolate), which had to be ingested within 10 min. A nurse not directly involved in the study distributed study chocolate to the patient.
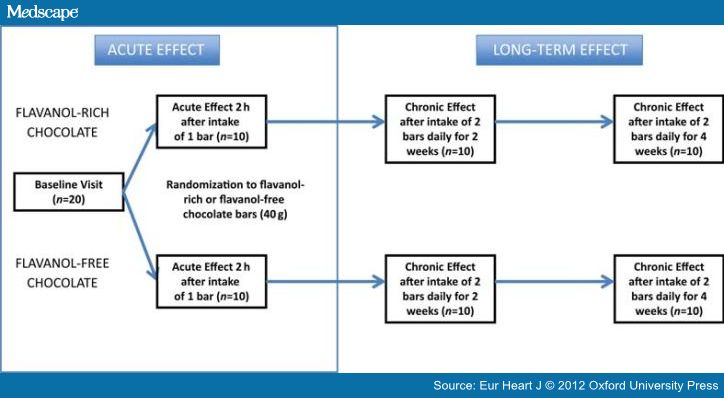
The study design is summarized in Figure 1. Primary endpoint of the study was endothelial function measured as FMD of the brachial artery. Secondary endpoints were baroreceptor function, platelet adhesion, and oxidative stress parameters. To assess the short-term effects, 2h after the baseline visit, endothelial and baroreceptor function and platelet adhesion measurements were repeated. Afterwards, all participants obtained a box with blinded FRC or CC bars, respectively, and were instructed to ingest one bar twice a day and to continue their normal daily diet. Endothelial, platelet, and baroreceptor functions were reassessed at 2 and 4 weeks to assess the longer-term effect. Measurements were performed after overnight fasting (at least 8 h) to assess thoroughly the long-term effects.
Subjects
Twenty-two patients with stable CHF (NYHA ≥ II) and ejection fraction <50% have been randomized. Exclusion criteria were: decompensated HF, unstable angina pectoris, smoking, creatinine >200 µmol/L, alanine aminotransferase or aspartate aminotransferase >150 IU, diabetes mellitus, obesity (body mass index >30 kg/m2), symptomatic hypotension, BP > 160/100 mmHg, known allergies to compounds of study chocolate or placebo, respectively, history of gastric ulcer or bleeding, venous thrombosis or pulmonary embolism, history of infectious disease or systemic inflammatory diseases, malignant tumours (unless cured or in remission for more than 5 years), concomitant vitamin supplements, as well as participation in another study within the last month. Two patients dropped out during follow-up (one patient withdrew consent because of personal reasons and one patient was excluded due to ventricular fibrillation, terminated by an internal defibrillator; this event was considered unrelated to the study protocol). Twenty patients were included into the final analysis.
Flavanol-rich and CC were prepared by Nestlé. Both were wrapped identically and randomization was done by an organization independent of the study group (InterCorNet, Zürich, Switzerland).
All patients gave signed informed consent. The study was performed at the University Hospital of Zurich, and the study protocol approved by the local Ethics Committee and conducted according to the Declaration of Helsinki. Patients were recruited from the HF outpatient clinic.
Experimental Protocol
All patients were instructed to refrain from flavanol-rich food for 24 h and fast for at least 8 h before baseline examinations, which were always performed in the morning. After a short clinical examination and blood sampling, baseline measurements were performed. Blood pressure was measured three times with a validated automatic BP device (OMRON Mit Elite Plus). The mean of the last two measurements was recorded. Following the first assessment, the participants were randomized to receive either 40 g of FRC or 28.4 g of CC (weight matched for fat and sugar content to the dark chocolate), which had to be ingested within 10 min. A nurse not directly involved in the study distributed study chocolate to the patient.
The study design is summarized in Figure 1. Primary endpoint of the study was endothelial function measured as FMD of the brachial artery. Secondary endpoints were baroreceptor function, platelet adhesion, and oxidative stress parameters. To assess the short-term effects, 2h after the baseline visit, endothelial and baroreceptor function and platelet adhesion measurements were repeated. Afterwards, all participants obtained a box with blinded FRC or CC bars, respectively, and were instructed to ingest one bar twice a day and to continue their normal daily diet. Endothelial, platelet, and baroreceptor functions were reassessed at 2 and 4 weeks to assess the longer-term effect. Measurements were performed after overnight fasting (at least 8 h) to assess thoroughly the long-term effects.
ResultsClinical CharacteristicsBaseline characteristics and medications of the study population are shown in Table 1. No significant difference was found between the two groups with the exception of a slightly lower plasma potassium in the group assigned to FRC (4.0 ± 0.2 and 4.2 ± 0.3, P = 0.05, respectively). Risk factor distribution was similar between the groups: history of arterial hypertension (FRC 2/10 and CC 3/10), dyslipidaemia (FRC 7/10, CC 5/10), and positive family history for cardiovascular disease (FRC 7/10, CC 6/10). According to the protocol, patients with diabetes mellitus and smokers were not included. Patients remained clinically stable during the study with no HF decompensation noted as also reflected by unchanged pro-B-natriuretic peptide levels (from 898.6 ± 1084.7 to 743.5 ± 1059.3 ng/L after FRC and from 667.0 ± 443.5 to 684.5 ± 513.7 ng/L after CC). Weight remained stable during the 4-week course of daily chocolate ingestion (76.7 ± 18.8–76.9 ± 18.7 and 76.8 ± 11.6–77.3 ± 11.4 kg, respectively).
Blood Pressure and Heart RateSystolic and diastolic BP and HR were not affected in the short and in the longer term (Table 2 andTable 3). Heart rate was rather low in this patient group, reflecting the appropriate use of β-blockers in this population.
Laboratory ParametersIn the group receiving cocoa-liquor-free chocolate, there was a significant decrease in insulin-sensitivity as assessed by the quantitative insulin sensitivity check index (QUICKI; Table 1 and Table 3), interestingly, an effect not seen in the FRC group. Otherwise, both FRC and cocoa-liquor-free CC had no immediate- or longer-term effects on laboratory parameters. There has been no acute or chronic impact on inflammatory a on oxidative stress markers, including total antioxidative capacity, ferric-reducing antioxidative capacity, or isoprostanes (Table 2 and Table 3).
The slight but statistically non-significant higher plasma levels of high-sensitivity C-reactive protein in the control group throughout the study can be attributed to one patient with elevated C-reactive protein levels. However, exclusion of this particular patient had no significant influence on the primary outcome.
Polyphenol Plasma LevelsThere was a significant increase in plasma polyphenols after ingestion of FRC, when compared with cocoa-liquor-free CC. Epicatechin concentration increased (from below detection limit to 0.69 ± 0.28 μM, P < 0.001 for intra- and between-group changes), whereas no plasma epicatechin were detectable before and after CC. However, in the FRC group (−)-epicatechin metabolites were only detected in the short term (2 h after ingestion) but not at the end of the 4-week treatment period (12 h after the last ingestion) (Table 2).
Flow-mediated Dilatation of the Brachial ArteryBaseline brachial artery diameter and baseline FMD were similar in both groups. Two hours after ingestion of 40 g of FRC, FMD increased from 4.98 ± 1.95 to 5.98 ± 2.32% (P = 0.045 and 0.02 for between groups), whereas the 28.4 g of CC showed no effect (from 5.06 ± 2.29 to 4.47 ± 1.5%; P = 0.44). Similarly, chronic daily intake of 80 g of FRC resulted in a significant amelioration of endothelial dysfunction both after 2 (from 4.98 ± 1.95 to 5.82 ± 1.54%; P = 0.045 and 0.33 for between groups) and after 4 weeks (from 4.98 ± 1.95 to 6.86 ± 1.76%; P = 0.027 and 0.004 for between groups), despite a 12 h refrain from flavanol-rich food before the follow-up measurements of FMD. Again, CC did not change FMD over the entire time course of up to 4 weeks (Figure 2). In the ANCOVA model to assess the effect of FRC while correcting for the baseline FMD values, the between-group comparison after 4 weeks is even more pronounced (P < 0.0001). Nitroglycerin-induced endothelial-independent vasodilatation was not different between the groups at all time (Table 2 and Table 3); additionally, reactive hyperaemia was not different between visits or within the treatment groups (data not shown). In addition to the improvement in endothelial function, FRC significantly increased baseline brachial artery diameter 2 h after ingestion (from 5.2 ± 1.2 to 5.4 ± 1.1 mm; P = 0.001 and P = 0.01 for between groups), while in the control group, the baseline diameter did not change (from 5.4 ± 0.8 to 5.4 ± 0.8 mm, respectively; P = 0.10).
(Enlarge Image)
Figure 2.
Effect of flavanol-rich and control chocolate, respectively endothelial function (measured by FMD). Two hours after ingestion of flavanol-rich chocolate, FMD increased from 4.98 ± 1.95 to 5.98 ± 2.32% whereas the control chocolate showed no significant effect (from 5.06 ± 2.29 to 4.47 ± 1.5%). Similarly, chronic daily intake of 80 g of flavanol-rich chocolate resulted in a significant amelioration of endothelial dysfunction after 4 weeks (from 4.98 ± 1.95 to 6.86 ± 1.76%). *P < 0.05.
Baroreceptor FunctionFlavanol-rich chocolate as well as cocoa-liquor-free CC did not significantly influence baroreceptor function in patients with HF. There were no acute and chronic changes in baroreceptor sensitivity in both the high- and low-frequency ranges (Table 2 and Table 3).
Platelet FunctionFlavanol-rich chocolate intake acutely improved platelet function. Two hours after chocolate intake, platelet adhesion was significantly reduced from 3.9 ± 1.3 to 3.0 ± 1.3% (P = 0.03 and 0.05 for between groups), whereas no change could be observed in the control group (from 3.3 ± 1.9 to 3.5 ± 1.7%, respectively; Figure 3). However, no significant effect of FRC on platelet adhesion was found at 4 weeks after chronic ingestion of FRC after a 12 h refrain period from flavanol-rich food (from 3.9 ± 1.3 to 4.1 ± 1.5%; P = 0.70 and P = 0.43 for between groups; Table 3).
(Enlarge Image)
Figure 3.
Acute effect of flavanol-rich and control chocolate, respectively, on platelet adhesion. P = 0.03 for flavanol-rich chocolate after 2 h compared with baseline.
Blood Pressure and Heart RateSystolic and diastolic BP and HR were not affected in the short and in the longer term (Table 2 andTable 3). Heart rate was rather low in this patient group, reflecting the appropriate use of β-blockers in this population.
Laboratory ParametersIn the group receiving cocoa-liquor-free chocolate, there was a significant decrease in insulin-sensitivity as assessed by the quantitative insulin sensitivity check index (QUICKI; Table 1 and Table 3), interestingly, an effect not seen in the FRC group. Otherwise, both FRC and cocoa-liquor-free CC had no immediate- or longer-term effects on laboratory parameters. There has been no acute or chronic impact on inflammatory a on oxidative stress markers, including total antioxidative capacity, ferric-reducing antioxidative capacity, or isoprostanes (Table 2 and Table 3).
The slight but statistically non-significant higher plasma levels of high-sensitivity C-reactive protein in the control group throughout the study can be attributed to one patient with elevated C-reactive protein levels. However, exclusion of this particular patient had no significant influence on the primary outcome.
Polyphenol Plasma LevelsThere was a significant increase in plasma polyphenols after ingestion of FRC, when compared with cocoa-liquor-free CC. Epicatechin concentration increased (from below detection limit to 0.69 ± 0.28 μM, P < 0.001 for intra- and between-group changes), whereas no plasma epicatechin were detectable before and after CC. However, in the FRC group (−)-epicatechin metabolites were only detected in the short term (2 h after ingestion) but not at the end of the 4-week treatment period (12 h after the last ingestion) (Table 2).
Flow-mediated Dilatation of the Brachial ArteryBaseline brachial artery diameter and baseline FMD were similar in both groups. Two hours after ingestion of 40 g of FRC, FMD increased from 4.98 ± 1.95 to 5.98 ± 2.32% (P = 0.045 and 0.02 for between groups), whereas the 28.4 g of CC showed no effect (from 5.06 ± 2.29 to 4.47 ± 1.5%; P = 0.44). Similarly, chronic daily intake of 80 g of FRC resulted in a significant amelioration of endothelial dysfunction both after 2 (from 4.98 ± 1.95 to 5.82 ± 1.54%; P = 0.045 and 0.33 for between groups) and after 4 weeks (from 4.98 ± 1.95 to 6.86 ± 1.76%; P = 0.027 and 0.004 for between groups), despite a 12 h refrain from flavanol-rich food before the follow-up measurements of FMD. Again, CC did not change FMD over the entire time course of up to 4 weeks (Figure 2). In the ANCOVA model to assess the effect of FRC while correcting for the baseline FMD values, the between-group comparison after 4 weeks is even more pronounced (P < 0.0001). Nitroglycerin-induced endothelial-independent vasodilatation was not different between the groups at all time (Table 2 and Table 3); additionally, reactive hyperaemia was not different between visits or within the treatment groups (data not shown). In addition to the improvement in endothelial function, FRC significantly increased baseline brachial artery diameter 2 h after ingestion (from 5.2 ± 1.2 to 5.4 ± 1.1 mm; P = 0.001 and P = 0.01 for between groups), while in the control group, the baseline diameter did not change (from 5.4 ± 0.8 to 5.4 ± 0.8 mm, respectively; P = 0.10).
(Enlarge Image)
Figure 2.
Effect of flavanol-rich and control chocolate, respectively endothelial function (measured by FMD). Two hours after ingestion of flavanol-rich chocolate, FMD increased from 4.98 ± 1.95 to 5.98 ± 2.32% whereas the control chocolate showed no significant effect (from 5.06 ± 2.29 to 4.47 ± 1.5%). Similarly, chronic daily intake of 80 g of flavanol-rich chocolate resulted in a significant amelioration of endothelial dysfunction after 4 weeks (from 4.98 ± 1.95 to 6.86 ± 1.76%). *P < 0.05.
Baroreceptor FunctionFlavanol-rich chocolate as well as cocoa-liquor-free CC did not significantly influence baroreceptor function in patients with HF. There were no acute and chronic changes in baroreceptor sensitivity in both the high- and low-frequency ranges (Table 2 and Table 3).
Platelet FunctionFlavanol-rich chocolate intake acutely improved platelet function. Two hours after chocolate intake, platelet adhesion was significantly reduced from 3.9 ± 1.3 to 3.0 ± 1.3% (P = 0.03 and 0.05 for between groups), whereas no change could be observed in the control group (from 3.3 ± 1.9 to 3.5 ± 1.7%, respectively; Figure 3). However, no significant effect of FRC on platelet adhesion was found at 4 weeks after chronic ingestion of FRC after a 12 h refrain period from flavanol-rich food (from 3.9 ± 1.3 to 4.1 ± 1.5%; P = 0.70 and P = 0.43 for between groups; Table 3).
(Enlarge Image)
Figure 3.
Acute effect of flavanol-rich and control chocolate, respectively, on platelet adhesion. P = 0.03 for flavanol-rich chocolate after 2 h compared with baseline.
Discussion
In the present study, we, for the first time, report a significant and specific effect of commercially available FRC on endothelial and platelet function, in patients with CHF. Interestingly, chocolate not only improved this important cardiovascular surrogate marker acutely, but even more so, after longer-term ingestion for up to 4 weeks. Such a vascular positive effect of an orally available molecule is not trivial in CHF as unexpectedly statins proved to be ineffective in this patient population.[17,18]
While most studies, so far, investigated only the acute effects of FRC on endothelial function,[1] we here report long-term effects with daily ingestion of FRC using a double-blind randomized design, rarely applied in nutritional research. In addition, this is the first study on the effect of chocolate in patients with advanced heart disease such as CHF. Of note, CHF is associated with endothelial dysfunction, a condition confirmed in our patient population. Indeed, FMD averaged about 4%, which is markedly lower than that observed in healthy controls.[25] The molecular mechanisms of endothelial dysfunction in CHF might involve increased levels of cytokines, impaired endothelial-receptor-signal transduction pathways, and increased angiotensin-converting enzyme activity.[26–29] Furthermore, neurohumoral activation and increased levels of endothelium-derived vasoconstrictors occurs in CHF.[30] In addition, CHF is associated with enhanced generation of reactive oxygen species and oxidized LDL, further counteracting vasodilator properties of NO. Therefore, the fact that cocoa polyphenols improve endothelial function by increasing NO synthase (NOS) activity and by exerting antioxidative capacity might be of importance for HF patients, especially as there is a strong association between endothelial dysfunction and cardiovascular morbidity and mortality in these patients.[10]Finally, CHF patients, particularly at advanced stages, are prone to weight loss, anaemia, and cachexia, making nutritional issues important in the management of such patients.
In our study, ingestion of FRC was followed by a marked and significant increase in (−)-epicatechin plasma concentrations. In parallel, FMD improved significantly in the flavanol, but not in the control group. This effect likely involves increased NO bioavailability, since it is reduced in CHF,[31] and ingestion of cocoa high in flavanols rapidly enhances the pool of bioactive NO and improves FMD in patients with hypertension or diabetes.[15,32] Furthermore, after the infusion of L-NMMA, an inhibitor of the NO synthesis, the increase in plasma NO levels as well as the amelioration of endothelial dysfunction associated with cocoa are blunted.[32] Moreover, a diet high in flavanols has been associated with a high urinary excretion of NO metabolites[33] and purified (−)-epicatechin has been shown to mimic the endothelial effects of flavanol-rich cocoa.[33] In the short term, flavanols inhibit the inactivation of NO by free radicals via inhibition of NADPH oxidase, while in the long term, they seem to be able to express higher levels of protein eNOS.[34] Furthermore, pure (−)-epicatechin ingestion not only augments NO bioavailability, but also reduces the plasma levels of endothelin-1, a potent endothelium-derived vasoconstrictor.[35]
Besides their effects on endothelial NOS expression, cocoa flavanols also exert antioxidant effects in vitro, which could contribute to the results of our study. In humans, it has been shown that cocoa is able to counteract lipid peroxidation, thus lowering the levels of plasma F2-isoprostanes, important markers of in vivo lipid peroxidation,[36] as well as plasma levels of oxLDL,[37] and increases overall antioxidant capacity.[38] Although not obvious in the current study, we showed that in young healthy smokers, the same commercially available chocolate as used in the present study was able not only to improve endothelial function but also to improve antioxidant status.[39] We also evaluated the effect of the same commercially available chocolate on cardiac transplant recipients, where we demonstrated a reduction in oxidative stress, as assessed by plasma isoprostanes; this was paralleled by coronary vasodilatation, improvement in coronary vascular function, and decreased platelet adhesion.[16]
Beyond the acute effects on endothelial function, the sustained and even more pronounced effects of chronic cocoa ingestion were remarkable. Indeed, endothelial function was further improved after 2 and particularly after 4 weeks of daily ingestion of 80 g of FRC. It is of note that endothelial function measurements were performed in the morning after overnight fasting; thus, an acute effect of chocolate in these measurements can be excluded. Indeed, in line with this assumption, both at 2 and 4 weeks, (−)-epicatechin and its methyl metabolites were no longer detectable in plasma at the time of vascular function studies. Therefore, chronic flavanol supplementation must have changed the biology of the brachial artery and endothelial cells, in particular in the CHF patients studied. Although, we do not have a mechanistic prove, flavanols most likely must have induced the expression of endothelial NOS, an effect that was sustained beyond the short half-life of these cocoa-derived nutrients. In line with this interpretation, brachial artery diameter increased 2h after ingestion of FRC. Furthermore, plasma levels of oxidative stress markers as well as of C-reactive protein were similar at 2 and 4 weeks as they had been at baseline excluding a major contribution of reactive oxidant species. Finally, endothelium-independent relaxations to nitroglycerin were unaffected by the dietary intervention.
The improvement in platelet function shortly after cocoa ingestion confirms our previous studies in young healthy smokers[39] and heart transplant recipients.[16] However, we were not able to show any long-term effect after 2 or 4 weeks. This may be due to the fact that blood samples were collected after an overnight fast, and thus, the polyphenols had already been metabolized and excreted as reflected by the lack of detection of these substances in the blood samples. Our findings are not surprising, since platelets are anucleated cells and hence unable to induce protein production, for instance, an increased transcription and translation of endothelial NOS expression. Hence, it appears that flavanols can activate NO release from platelets as previously described,[40] but—in contrast to endothelial cells—are unable to exert sustained effects in these anucleated cells.
Neurohumoral activation, in particular activation of the sympathetic nervous system, is a hallmark of CHF. Thus, we further investigated the effect of FRC on baroreceptor function by the α-coefficient method. However, no effect of the dietary intervention has been noted, neither in the short nor in the long term. This is surprising, since NO has been involved in baroreceptor signalling.[41] An explanation might be the use of β-blocking agents in all of our patients according to guidelines, thus masking a possible effect of FRC. Alternatively, the limited number of observations may also contribute to the negative findings, as baroreflex function was only measured in 11 patients.
Epidemiological and small intervention studies suggest a small, but distinct BP-lowering effect of chocolate consumption.[2,3,42,43] However, these studies were performed in patients with elevated or mildly elevated BP. Moreover, the effect of BP lowering was higher in subjects with higher baseline BP.[43] As it is typical in CHF, baseline BP of our patients was low and averaged 110/65 mmHg. We did not observe any relevant effect of FRC consumption on systolic or diastolic BP, neither acutely nor after 2 and 4 weeks, despite a substantial increase in plasma epicatechin levels and that of its metabolites. This might be explained by the low baseline BP as well as by the fact that antihypertensive drugs had been used. Intervention studies demonstrated improved insulin sensitivity after chocolate consumption, especially in hypertensives.[14,42] Interestingly, in this study, we observed a decrease in insulin sensitivity after 4 weeks in the control group, a decrease not seen in patients consuming FRC. This may potentially point towards an additional beneficial effect of FRC in CHF patients. It is of note that despite the high caloric load of our commercially available FRC, no weight gain and no change in blood lipids were noted.
There are some limitations of the study. We did not control for habitual food intake, especially for other cocoa products. Furthermore, patients were free to schedule study chocolate intake; thus, other foods might have influenced bioavailability. Although we think it is unlikely, we cannot exclude that the results are biased by the individuals' diet. We are aware that our results are based on a rather small sample size; thus, effects on secondary endpoints such as BP, oxidative stress parameters, and others might not have been detected.
In conclusion:
This is the first study demonstrating beneficial cardiovascular effects of commercially available FRC in patients with CHF. Flavanol-rich chocolate not only led to peripheral vasodilatation, improvement in endothelial function, and enhancement in platelet function shortly after chocolate ingestion but also to an amelioration in endothelial function in the long term after 2 and 4 weeks of daily chocolate ingestion. It is of note that endothelial function was improved on top of optimal medical treatment with drugs known to improve vascular function alone.
While most studies, so far, investigated only the acute effects of FRC on endothelial function,[1] we here report long-term effects with daily ingestion of FRC using a double-blind randomized design, rarely applied in nutritional research. In addition, this is the first study on the effect of chocolate in patients with advanced heart disease such as CHF. Of note, CHF is associated with endothelial dysfunction, a condition confirmed in our patient population. Indeed, FMD averaged about 4%, which is markedly lower than that observed in healthy controls.[25] The molecular mechanisms of endothelial dysfunction in CHF might involve increased levels of cytokines, impaired endothelial-receptor-signal transduction pathways, and increased angiotensin-converting enzyme activity.[26–29] Furthermore, neurohumoral activation and increased levels of endothelium-derived vasoconstrictors occurs in CHF.[30] In addition, CHF is associated with enhanced generation of reactive oxygen species and oxidized LDL, further counteracting vasodilator properties of NO. Therefore, the fact that cocoa polyphenols improve endothelial function by increasing NO synthase (NOS) activity and by exerting antioxidative capacity might be of importance for HF patients, especially as there is a strong association between endothelial dysfunction and cardiovascular morbidity and mortality in these patients.[10]Finally, CHF patients, particularly at advanced stages, are prone to weight loss, anaemia, and cachexia, making nutritional issues important in the management of such patients.
In our study, ingestion of FRC was followed by a marked and significant increase in (−)-epicatechin plasma concentrations. In parallel, FMD improved significantly in the flavanol, but not in the control group. This effect likely involves increased NO bioavailability, since it is reduced in CHF,[31] and ingestion of cocoa high in flavanols rapidly enhances the pool of bioactive NO and improves FMD in patients with hypertension or diabetes.[15,32] Furthermore, after the infusion of L-NMMA, an inhibitor of the NO synthesis, the increase in plasma NO levels as well as the amelioration of endothelial dysfunction associated with cocoa are blunted.[32] Moreover, a diet high in flavanols has been associated with a high urinary excretion of NO metabolites[33] and purified (−)-epicatechin has been shown to mimic the endothelial effects of flavanol-rich cocoa.[33] In the short term, flavanols inhibit the inactivation of NO by free radicals via inhibition of NADPH oxidase, while in the long term, they seem to be able to express higher levels of protein eNOS.[34] Furthermore, pure (−)-epicatechin ingestion not only augments NO bioavailability, but also reduces the plasma levels of endothelin-1, a potent endothelium-derived vasoconstrictor.[35]
Besides their effects on endothelial NOS expression, cocoa flavanols also exert antioxidant effects in vitro, which could contribute to the results of our study. In humans, it has been shown that cocoa is able to counteract lipid peroxidation, thus lowering the levels of plasma F2-isoprostanes, important markers of in vivo lipid peroxidation,[36] as well as plasma levels of oxLDL,[37] and increases overall antioxidant capacity.[38] Although not obvious in the current study, we showed that in young healthy smokers, the same commercially available chocolate as used in the present study was able not only to improve endothelial function but also to improve antioxidant status.[39] We also evaluated the effect of the same commercially available chocolate on cardiac transplant recipients, where we demonstrated a reduction in oxidative stress, as assessed by plasma isoprostanes; this was paralleled by coronary vasodilatation, improvement in coronary vascular function, and decreased platelet adhesion.[16]
Beyond the acute effects on endothelial function, the sustained and even more pronounced effects of chronic cocoa ingestion were remarkable. Indeed, endothelial function was further improved after 2 and particularly after 4 weeks of daily ingestion of 80 g of FRC. It is of note that endothelial function measurements were performed in the morning after overnight fasting; thus, an acute effect of chocolate in these measurements can be excluded. Indeed, in line with this assumption, both at 2 and 4 weeks, (−)-epicatechin and its methyl metabolites were no longer detectable in plasma at the time of vascular function studies. Therefore, chronic flavanol supplementation must have changed the biology of the brachial artery and endothelial cells, in particular in the CHF patients studied. Although, we do not have a mechanistic prove, flavanols most likely must have induced the expression of endothelial NOS, an effect that was sustained beyond the short half-life of these cocoa-derived nutrients. In line with this interpretation, brachial artery diameter increased 2h after ingestion of FRC. Furthermore, plasma levels of oxidative stress markers as well as of C-reactive protein were similar at 2 and 4 weeks as they had been at baseline excluding a major contribution of reactive oxidant species. Finally, endothelium-independent relaxations to nitroglycerin were unaffected by the dietary intervention.
The improvement in platelet function shortly after cocoa ingestion confirms our previous studies in young healthy smokers[39] and heart transplant recipients.[16] However, we were not able to show any long-term effect after 2 or 4 weeks. This may be due to the fact that blood samples were collected after an overnight fast, and thus, the polyphenols had already been metabolized and excreted as reflected by the lack of detection of these substances in the blood samples. Our findings are not surprising, since platelets are anucleated cells and hence unable to induce protein production, for instance, an increased transcription and translation of endothelial NOS expression. Hence, it appears that flavanols can activate NO release from platelets as previously described,[40] but—in contrast to endothelial cells—are unable to exert sustained effects in these anucleated cells.
Neurohumoral activation, in particular activation of the sympathetic nervous system, is a hallmark of CHF. Thus, we further investigated the effect of FRC on baroreceptor function by the α-coefficient method. However, no effect of the dietary intervention has been noted, neither in the short nor in the long term. This is surprising, since NO has been involved in baroreceptor signalling.[41] An explanation might be the use of β-blocking agents in all of our patients according to guidelines, thus masking a possible effect of FRC. Alternatively, the limited number of observations may also contribute to the negative findings, as baroreflex function was only measured in 11 patients.
Epidemiological and small intervention studies suggest a small, but distinct BP-lowering effect of chocolate consumption.[2,3,42,43] However, these studies were performed in patients with elevated or mildly elevated BP. Moreover, the effect of BP lowering was higher in subjects with higher baseline BP.[43] As it is typical in CHF, baseline BP of our patients was low and averaged 110/65 mmHg. We did not observe any relevant effect of FRC consumption on systolic or diastolic BP, neither acutely nor after 2 and 4 weeks, despite a substantial increase in plasma epicatechin levels and that of its metabolites. This might be explained by the low baseline BP as well as by the fact that antihypertensive drugs had been used. Intervention studies demonstrated improved insulin sensitivity after chocolate consumption, especially in hypertensives.[14,42] Interestingly, in this study, we observed a decrease in insulin sensitivity after 4 weeks in the control group, a decrease not seen in patients consuming FRC. This may potentially point towards an additional beneficial effect of FRC in CHF patients. It is of note that despite the high caloric load of our commercially available FRC, no weight gain and no change in blood lipids were noted.
There are some limitations of the study. We did not control for habitual food intake, especially for other cocoa products. Furthermore, patients were free to schedule study chocolate intake; thus, other foods might have influenced bioavailability. Although we think it is unlikely, we cannot exclude that the results are biased by the individuals' diet. We are aware that our results are based on a rather small sample size; thus, effects on secondary endpoints such as BP, oxidative stress parameters, and others might not have been detected.
In conclusion:
This is the first study demonstrating beneficial cardiovascular effects of commercially available FRC in patients with CHF. Flavanol-rich chocolate not only led to peripheral vasodilatation, improvement in endothelial function, and enhancement in platelet function shortly after chocolate ingestion but also to an amelioration in endothelial function in the long term after 2 and 4 weeks of daily chocolate ingestion. It is of note that endothelial function was improved on top of optimal medical treatment with drugs known to improve vascular function alone.