To Statin or not to Statin ? That is the question !
Statins are one of the new wonder drugs.
Which makes them controversial.
But some experts think they are so good that you have to look for a not be on a statin.
Statins lower cholesterol.
Statins prevent cancer.
Statins prevent heart attacks and strokes.
Statins make people Live longer !
Statins might make cardiac patients less depressed - click here
Which makes them controversial.
But some experts think they are so good that you have to look for a not be on a statin.
Statins lower cholesterol.
Statins prevent cancer.
Statins prevent heart attacks and strokes.
Statins make people Live longer !
Statins might make cardiac patients less depressed - click here
Statins users have less cancer deaths of all kinds ( in Denmark )
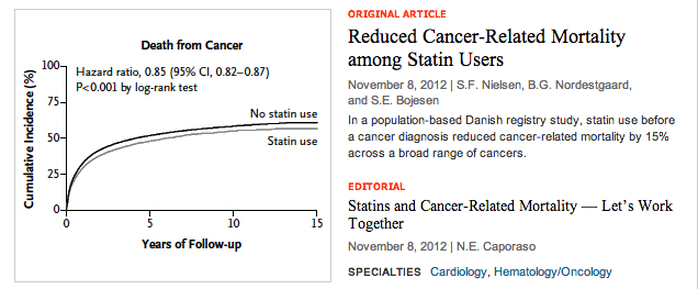
NEJM 7 NOV 2012
7 Nov 2012
A study published in the New England Journal of Medicine shows that Danish people who take a statin drug are about 15 % less likely to die of cancer.
So a heart attack prevention drug now also lowers cancer deaths.
Possibly because tumors need cholesterol to make the cell membranes they need for unrestrained growth. So less available cholesterol means less cancer cells.
Using Danish national registries, researchers identified nearly 300,000 adults aged 40 and older who were diagnosed with cancer between 1995 and 2007. Of these, 6% were regular statin users before diagnosis.
During a median 2.6 years' follow-up, cancer-related mortality was reduced by 15% among statin users versus nonusers, with reductions observed for 13 types of cancer. All-cause mortality was similarly reduced among statin users. ( Which is a quirky statistical way of saying that statin users die less of "everything".)
Patients who are already taking statins (and tolerating them) at the time of cancer diagnosis should continue taking them."
For more information on how statins prevent cancer click here
For an article on how statins can improve the prognosis of prostate cancer click here
Statins as a Treatment for Prostate Cancer
.Statins seem to be beneficial for many forms of cancer. Click here to see how they can improve the prognosis of prostate cancer .
In men who took a statin after they were diagnosed with prostate cancer, cancer-specific and overall mortality rates were lower than in men who did not take a statin, a nationwide Danish registry study has found.
"Increasing evidence indicates that the use of statins may delay prostate cancer (PC) progression," write the authors, led by Signe Benzon Larsen, PhD, Danish Cancer Society Research Center, Copenhagen, Denmark.
"Our study adds to the increasing evidence that statin use is associated with reduced PC mortality," the investigators add.
The study was published online August 14 in the Journal of Clinical Oncology.
In men who took a statin after they were diagnosed with prostate cancer, cancer-specific and overall mortality rates were lower than in men who did not take a statin, a nationwide Danish registry study has found.
"Increasing evidence indicates that the use of statins may delay prostate cancer (PC) progression," write the authors, led by Signe Benzon Larsen, PhD, Danish Cancer Society Research Center, Copenhagen, Denmark.
"Our study adds to the increasing evidence that statin use is associated with reduced PC mortality," the investigators add.
The study was published online August 14 in the Journal of Clinical Oncology.
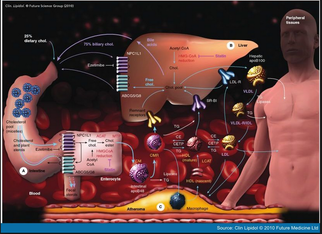
Cholesterol lowering effect of statins
Diet and exercise are the usual first steps in lowering cholesterol and in preventing heart attacks and strokes. Everyone should do a bit of exercise everyday - opinions vary from 7 minutes of very intense exercise, to 45 min of fast walking. But any exercise is better than no exercise.
Diet is the next mainstay. Some heart healthy diets will soon be listed on another page on this website.
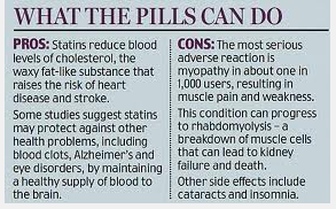
By combining diet and exercise you can lower your cholesterol by about 15 % in theory, and by about 8% in practice. By popping a statin pill every day you can lower your cholesterol by 50%. All for about the price of a latte a day. And on the bright side, you may even get some muscle aches, to make you feel like you have been exercising.
Diet is the next mainstay. Some heart healthy diets will soon be listed on another page on this website.
By combining diet and exercise you can lower your cholesterol by about 15 % in theory, and by about 8% in practice. By popping a statin pill every day you can lower your cholesterol by 50%. All for about the price of a latte a day. And on the bright side, you may even get some muscle aches, to make you feel like you have been exercising.
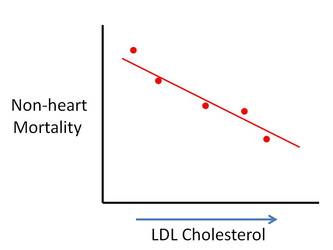
Statins make you live longer
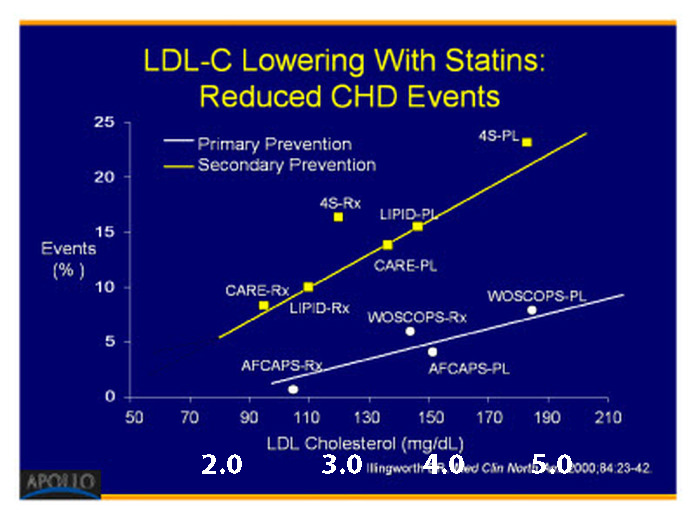
The above graph shows that whatever your "bad cholesterol" or "LDL" cholesterol is, lowering it is a good idea. As low as you can get it.
If you can get your LDL below 2 your arteries even starting cleaning themselves out over time instead of getting more gummed up !
If you can get your LDL below 2 your arteries even starting cleaning themselves out over time instead of getting more gummed up !
Pleiotropic Effects of Statins (that means they 'do a lot of stuff' )
Question : Are the pleiotropic effects of statins, including the anti-inflammatory effects, proportional to the degree of lipid lowering?
Answer :
Potent inhibitors of cholesterol biosynthesis, statins have been proven to be beneficial in both primary and secondary prevention of CVD. However, the overall benefits of statins, as observed in clinical trials, appear to be greater than what might be expected from changes in lipid levels alone, suggesting effects beyond cholesterol lowering.
Mounting evidence suggests that some of the cholesterol independent or pleiotropic effects of statins include improvement in :
- endothelial function ( they are "good for blood vessels")
- reduction of oxidative stress ( they prevent "cell damage")
- inhibition of platelet aggregation ( less blood "clot-ability")
- stabilization of atherosclerotic plaques by attenuation of the inflammatory response. ( they make hardening of the arteries less evil )
In addition, statins have been shown to have beneficial extrahepatic effects, including:
- enhancing immune function
- protecting the brain and nervous system
- improving renal function
- reducing serum uric acid levels
- improving bone mineralization.
Although proof in appropriately designed trials is currently lacking, there is data to suggest that, in high-risk patient groups, the pleiotropic effects of statins may be partially responsible for the observed reduction of morbidity and mortality, and proportional to the degree of lipid lowering.
While this is all very exciting, it’s important to remember that although cholesterol-independent effects may be at play with statin therapy, LDL-C is a meddlesome metabolite, which raises havoc on our cardiovascular system in diverse and extensive ways. Therefore, LDL-C lowering needs to remain our priority in managing patients at risk for CVD, with goals less than 2.0 mmol/L in both moderate- and high-risk groups.
Click here for a link to the original medical journal article and the references.
Answer :
Potent inhibitors of cholesterol biosynthesis, statins have been proven to be beneficial in both primary and secondary prevention of CVD. However, the overall benefits of statins, as observed in clinical trials, appear to be greater than what might be expected from changes in lipid levels alone, suggesting effects beyond cholesterol lowering.
Mounting evidence suggests that some of the cholesterol independent or pleiotropic effects of statins include improvement in :
- endothelial function ( they are "good for blood vessels")
- reduction of oxidative stress ( they prevent "cell damage")
- inhibition of platelet aggregation ( less blood "clot-ability")
- stabilization of atherosclerotic plaques by attenuation of the inflammatory response. ( they make hardening of the arteries less evil )
In addition, statins have been shown to have beneficial extrahepatic effects, including:
- enhancing immune function
- protecting the brain and nervous system
- improving renal function
- reducing serum uric acid levels
- improving bone mineralization.
Although proof in appropriately designed trials is currently lacking, there is data to suggest that, in high-risk patient groups, the pleiotropic effects of statins may be partially responsible for the observed reduction of morbidity and mortality, and proportional to the degree of lipid lowering.
While this is all very exciting, it’s important to remember that although cholesterol-independent effects may be at play with statin therapy, LDL-C is a meddlesome metabolite, which raises havoc on our cardiovascular system in diverse and extensive ways. Therefore, LDL-C lowering needs to remain our priority in managing patients at risk for CVD, with goals less than 2.0 mmol/L in both moderate- and high-risk groups.
Click here for a link to the original medical journal article and the references.
"Number Needed To Treat" and what it means
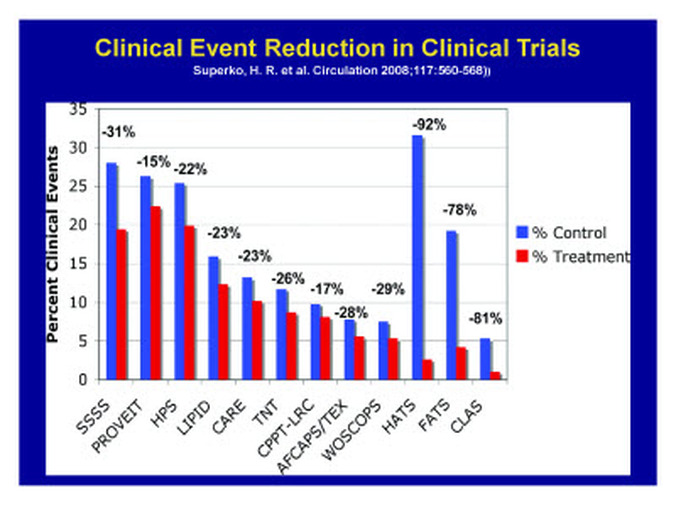
Clinical bottom line - How well do the statins work - the "number needed to treat" to make a difference.
Using BNF definitions of cardiovascular risk and extrapolated 10-year efficacy, the NNT of statins is 6 and below for risks of 40% and above, and 11 falling to 6 at risks of 20-40%.
What this means in plain English is that for high risk patients giving statins to six people will result in one heart attack or stroke prevented.
If you are at lower risk, then the 'number needed to treat' to prevent one adverse event drops to about 12. Which means that for every dozen middle risk people that get put on a statin, one won't have a heart attack they otherwise would have.
Them is pretty darn good odds. No wonder some cardiologists say that you have to look for reasons NOT to put a middle aged thick guy on a statin.
The evidence is that statins are effective in reducing heart attacks and stroke, both fatal and non-fatal.
This reduction occurred consistently in large randomised trials with event rates for the combined outcome of fatal or nonfatal heart attack or stroke over five years of 10 to 35%. This corresponds to a 10-year risk of 20 to 70%
Using BNF definitions of cardiovascular risk and extrapolated 10-year efficacy, the NNT of statins is 6 and below for risks of 40% and above, and 11 falling to 6 at risks of 20-40%.
What this means in plain English is that for high risk patients giving statins to six people will result in one heart attack or stroke prevented.
If you are at lower risk, then the 'number needed to treat' to prevent one adverse event drops to about 12. Which means that for every dozen middle risk people that get put on a statin, one won't have a heart attack they otherwise would have.
Them is pretty darn good odds. No wonder some cardiologists say that you have to look for reasons NOT to put a middle aged thick guy on a statin.
The evidence is that statins are effective in reducing heart attacks and stroke, both fatal and non-fatal.
This reduction occurred consistently in large randomised trials with event rates for the combined outcome of fatal or nonfatal heart attack or stroke over five years of 10 to 35%. This corresponds to a 10-year risk of 20 to 70%
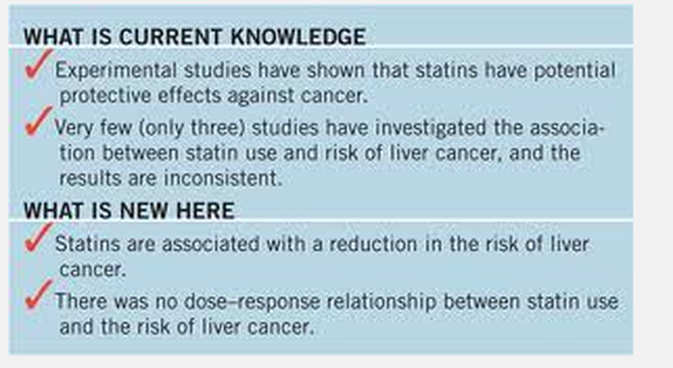
Statins are assoc. with decreased liver cancer...2012 data
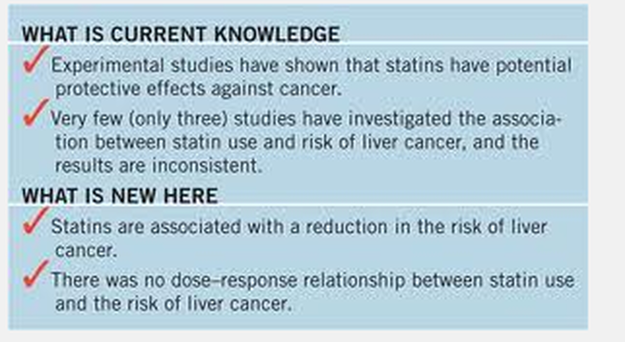
Statins and primary liver cancer:
a meta-analysis of observational studies
Pradelli, Danitza; Soranna, Davide; Scotti, Lorenza; Zambon, Antonella; Catapano, Alberico; Mancia, Giuseppe; La Vecchia, Carlo; Corrao, Giovanni
Abstract
Statins are among the most commonly prescribed drugs used to manage dyslipidemia. Hepatocellular carcinoma is the third leading cause of cancer mortality and its rates have recently been increasing in central and northern Europe and USA. To quantify the association between statin use and risk for HCC, we performed a meta-analysis of published studies. We conducted a MEDLINE search for observational studies reporting the association between exposure to statins and risk for incident liver cancer until March 2012. Fixed-effect and random-effect models were used to estimate summary relative risks (RR) and the corresponding 95% confidence intervals (CIs). Moreover, between-study heterogeneity and publication bias were assessed using adequate statistical tests. Five observational studies (two case-control and three cohort studies) based on 2574 cases of HCC were included. Statin treatment, compared with no treatment, was inversely related to HCC (summary RR=0.58; 95% CI 0.46-0.74). Between-study heterogeneity was significant (P<0.001) and numerically relevant (I2=65%). When only longest statin use was considered, the RR was 0.66 (95% CI 0.55-0.80). Influence analysis on the overall estimate showed that heterogeneity was largely because of one study; when omitting it, the I2 dropped to 27% (P=0.240), whereas the summary RR was only marginally modified (RR=0.52; 95% CI 0.44-0.62). There was no evidence of publication bias. This meta-analysis suggests a favorable effect of statins on HCC, in the absence, however, of a duration-risk relationship.
(C) 2012 Lippincott Williams & Wilkins, Inc.
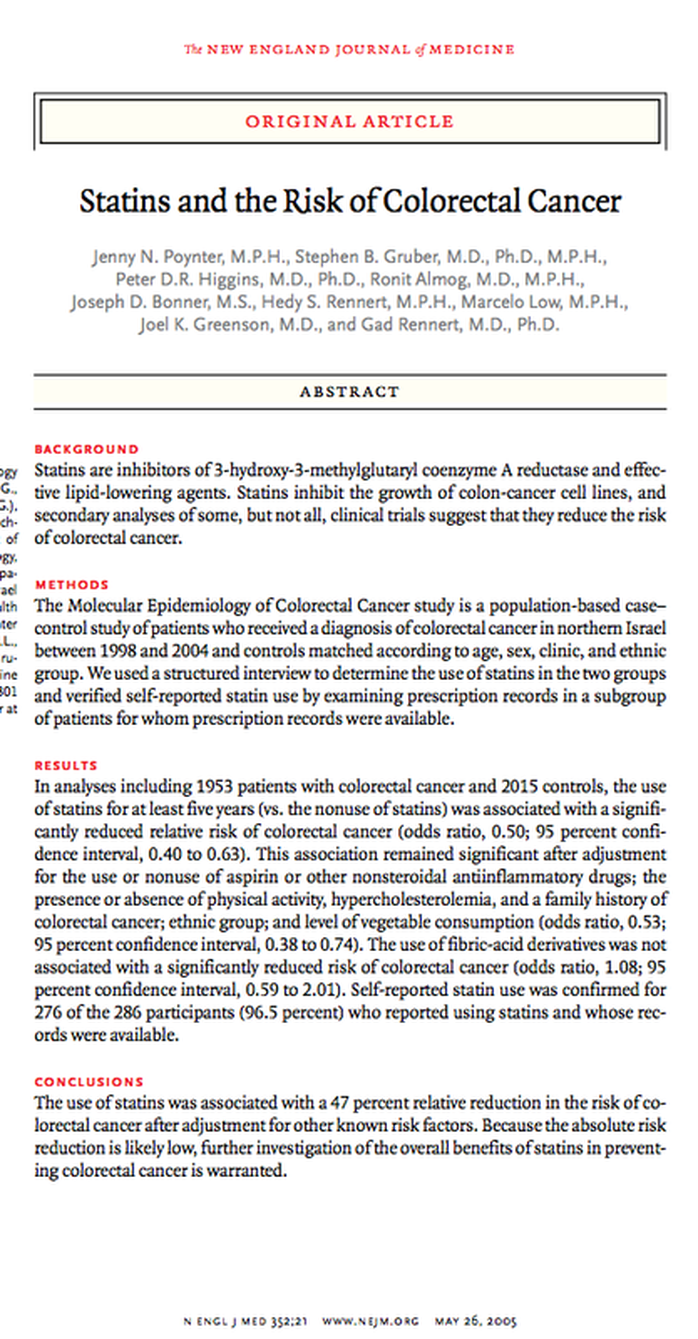
Statins cut colon cancer by almost 50 %
.
Should we put everyone on Statins ?

Statins prevent cancer
Statins prevent heart disease.
Does this mean that all middle -aged folk, even those without cardiovascular or cancer risk factors - should be on Statins ?
The answer is a very definite -" maybe" .
Remember, almost all the statin reviews have been for either cardiac problems or cancer prevention, or "all cause" mortality. Not too many consider all the benefits of statins put together.
Still, there is good evidence to at least think about putting everyone on a statin.
If you look at the page on "Cardiovascular Risk Stratification" you will see that all males 45 and over have a sixty percent chance of dying of heart disease someday. So even those with "no risk factors" are at risk.
It also makes sense that the higher your risk factors the more benefit you will get from a statin. If you have had six heart attacks and your cholesterol is twice normal, statins are a no brainer. If you are a 45 year old guy who plays hockey three times a week statins might still be a good idea. But because you are at so much less risk, the benefit of the statins are correspondingly less. But as seen below, they still may be worthwhile.
Statins prevent heart disease.
Does this mean that all middle -aged folk, even those without cardiovascular or cancer risk factors - should be on Statins ?
The answer is a very definite -" maybe" .
Remember, almost all the statin reviews have been for either cardiac problems or cancer prevention, or "all cause" mortality. Not too many consider all the benefits of statins put together.
Still, there is good evidence to at least think about putting everyone on a statin.
If you look at the page on "Cardiovascular Risk Stratification" you will see that all males 45 and over have a sixty percent chance of dying of heart disease someday. So even those with "no risk factors" are at risk.
It also makes sense that the higher your risk factors the more benefit you will get from a statin. If you have had six heart attacks and your cholesterol is twice normal, statins are a no brainer. If you are a 45 year old guy who plays hockey three times a week statins might still be a good idea. But because you are at so much less risk, the benefit of the statins are correspondingly less. But as seen below, they still may be worthwhile.
Statins for everyone ? ( ie should we give statins to everyone as "primary" prevention, in all people ?)

Statins for the primary prevention of cardiovascular disease.
Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Casas JP, Ebrahim S.
SourceDepartment of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, Keppel Street, London, UK, WC1E 7HT.
BACKGROUND:
Reducing high blood cholesterol, a risk factor for cardiovascular disease (CVD) events in people with and without a past history of coronary heart disease (CHD) is an important goal of pharmacotherapy. Statins are the first-choice agents. Previous reviews of the effects of statins have highlighted their benefits in people with coronary artery disease. The case for primary prevention, however, is less clear.
OBJECTIVES:To assess the effects, both harms and benefits, of statins in people with no history of CVD.
SEARCH STRATEGY:To avoid duplication of effort, we checked reference lists of previous systematic reviews. We searched the Cochrane Central Register of Controlled Trials (Issue 1, 2007), MEDLINE (2001 to March 2007) and EMBASE (2003 to March 2007). There were no language restrictions.
SELECTION CRITERIA:Randomised controlled trials of statins with minimum duration of one year and follow-up of six months, in adults with no restrictions on their total low density lipoprotein (LDL) or high density lipoprotein (HDL) cholesterol levels, and where 10% or less had a history of CVD, were included.
DATA COLLECTION AND ANALYSIS:Two authors independently selected studies for inclusion and extracted data. Outcomes included all cause mortality, fatal and non-fatal CHD, CVD and stroke events, combined endpoints (fatal and non-fatal CHD, CVD and stroke events), change in blood total cholesterol concentration, revascularisation, adverse events, quality of life and costs. Relative risk (RR) was calculated for dichotomous data, and for continuous data pooled weighted mean differences (with 95% confidence intervals) were calculated.
MAIN RESULTS:Fourteen randomised control trials (16 trial arms; 34,272 participants) were included. Eleven trials recruited patients with specific conditions (raised lipids, diabetes, hypertension, microalbuminuria). All-cause mortality was reduced by statins (RR 0.83, 95% CI 0.73 to 0.95) as was combined fatal and non-fatal CVD endpoints (RR 0.70, 95% CI 0.61 to 0.79). Benefits were also seen in the reduction of revascularisation rates (RR 0.66, 95% CI 0.53 to 0.83). Total cholesterol and LDL cholesterol were reduced in all trials but there was evidence of heterogeneity of effects. There was no clear evidence of any significant harm caused by statin prescription or of effects on patient quality of life.
AUTHORS' CONCLUSIONS: Although reductions in all-cause mortality, composite endpoints and revascularisations were found with no excess of adverse events, there was evidence of selective reporting of outcomes, failure to report adverse events and inclusion of people with cardiovascular disease. Only limited evidence showed that primary prevention with statins may be cost effective and improve patient quality of life. Caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk.
Can people with fatty liver take statins ?

From the Family Physicians Inquiries Network
Evidence-based answer
Patients with steatohepatitis who take HMG Co-A reductase inhibitors (statins) lower their elevated liver enzymes and show evidence of improvement in fatty liver on follow-up imaging (strength of recommendation [SOR]: C, based on very small, short-term prospective studies).
Statins do not further increase transaminase levels for patients with pre-existing transaminase elevations (SOR: B, based on 2 retrospective cohort studies). However, for patients with decompensated liver disease or advanced cirrhosis, balance the benefits of statins against the risks (SOR: C, based on expert opinion).
CLINICAL COMMENTARY
Remain cautious in prescribing statins for those with nonalcoholic steatohepatitis
Robert C. Oh, MD, MPH Department of Family Medicine, Tripler Army Medical Center, Honolulu, Hawaii
It is encouraging to see that statins may not worsen nonalcoholic steatohepatitis (NASH) and can potentially improve the process. However, these conclusions are supported by small clinical trials, and clinicians should remain cautious in prescribing statins for patients with NASH.
Importantly, if liver enzyme elevations are revealed during baseline examinations, consider statins only if a systematic work-up is unrevealing and suggests only NASH.7-9 However, I generally avoid statins for those with more than mild to moderate elevations (greater than 100).
Before starting statins, I inform patients of the small but potential risk of worsening hepatotoxicity and the importance of close follow-up. If the patient is agreeable, obtaining hepatic enzymes after each statin dose change and periodically after cholesterol goals are achieved is integral in the successful management of the NASH patient requiring statin therapy.
Evidence-based answer
Patients with steatohepatitis who take HMG Co-A reductase inhibitors (statins) lower their elevated liver enzymes and show evidence of improvement in fatty liver on follow-up imaging (strength of recommendation [SOR]: C, based on very small, short-term prospective studies).
Statins do not further increase transaminase levels for patients with pre-existing transaminase elevations (SOR: B, based on 2 retrospective cohort studies). However, for patients with decompensated liver disease or advanced cirrhosis, balance the benefits of statins against the risks (SOR: C, based on expert opinion).
CLINICAL COMMENTARY
Remain cautious in prescribing statins for those with nonalcoholic steatohepatitis
Robert C. Oh, MD, MPH Department of Family Medicine, Tripler Army Medical Center, Honolulu, Hawaii
It is encouraging to see that statins may not worsen nonalcoholic steatohepatitis (NASH) and can potentially improve the process. However, these conclusions are supported by small clinical trials, and clinicians should remain cautious in prescribing statins for patients with NASH.
Importantly, if liver enzyme elevations are revealed during baseline examinations, consider statins only if a systematic work-up is unrevealing and suggests only NASH.7-9 However, I generally avoid statins for those with more than mild to moderate elevations (greater than 100).
Before starting statins, I inform patients of the small but potential risk of worsening hepatotoxicity and the importance of close follow-up. If the patient is agreeable, obtaining hepatic enzymes after each statin dose change and periodically after cholesterol goals are achieved is integral in the successful management of the NASH patient requiring statin therapy.
Cochrane Collaboration Info

Statins for the primary prevention of cardiovascular disease
Taylor F, Ward K, Moore THM, Burke M, Davey Smith G, Casas JP, Ebrahim S
Published Online:
May 16, 2012
Cardiovascular disease (CVD) is ranked as the number one cause of mortality and is a major cause of morbidity world wide. Reducing high blood cholesterol which is a risk factor for CVD events is an important goal of medical treatment. Statins are the first-choice agents. Since the early statin trials were reported, several reviews of the effects of statins have been published highlighting their benefits particularly in people with a past history of CVD. However for people without a past history of CVD (primary prevention), the evidence is less clear. The aim of this systematic review is to assess the effects, both in terms of benefits and harms of statins for the primary prevention of CVD. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE until 2007. We found 14 randomised control trials with 16 trial arms (34,272 patients) dating from 1994 to 2006. All were randomised control trials comparing statins with usual care or placebo. Duration of treatment was minimum one year and with follow up of a minimum of six months.
All cause mortality. coronary heart disease and stroke events were reduced with the use of statins as was the need for revascularisations. Statin treatment reduced blood cholesterol. Taking statins did not increase the risk of adverse effects such as cancer. and few trials reported on costs or quality of life. This current systematic review highlights the shortcomings in the published trials and we recommend that caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk.
Taylor F, Ward K, Moore THM, Burke M, Davey Smith G, Casas JP, Ebrahim S
Published Online:
May 16, 2012
Cardiovascular disease (CVD) is ranked as the number one cause of mortality and is a major cause of morbidity world wide. Reducing high blood cholesterol which is a risk factor for CVD events is an important goal of medical treatment. Statins are the first-choice agents. Since the early statin trials were reported, several reviews of the effects of statins have been published highlighting their benefits particularly in people with a past history of CVD. However for people without a past history of CVD (primary prevention), the evidence is less clear. The aim of this systematic review is to assess the effects, both in terms of benefits and harms of statins for the primary prevention of CVD. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE until 2007. We found 14 randomised control trials with 16 trial arms (34,272 patients) dating from 1994 to 2006. All were randomised control trials comparing statins with usual care or placebo. Duration of treatment was minimum one year and with follow up of a minimum of six months.
All cause mortality. coronary heart disease and stroke events were reduced with the use of statins as was the need for revascularisations. Statin treatment reduced blood cholesterol. Taking statins did not increase the risk of adverse effects such as cancer. and few trials reported on costs or quality of life. This current systematic review highlights the shortcomings in the published trials and we recommend that caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk.