The Good, the Bad, and the Ugly ...

The Good
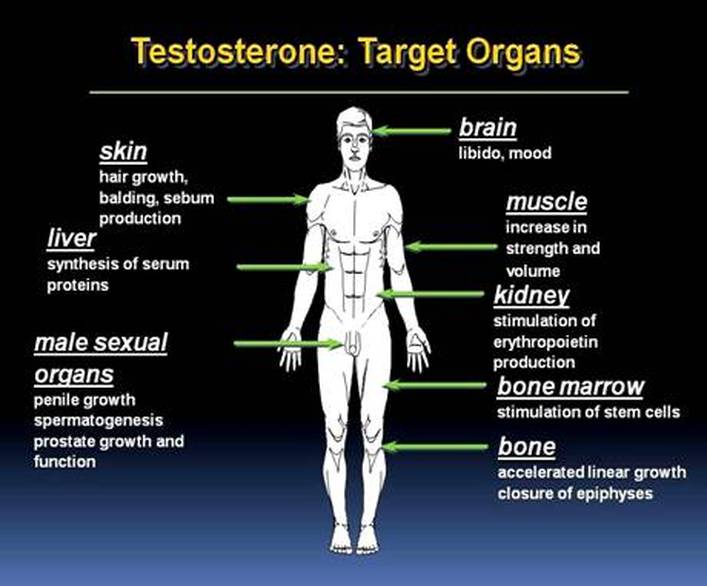
Testosterone is good for :
- osteoporosis
- anemia
- cholesterol
- heart disease
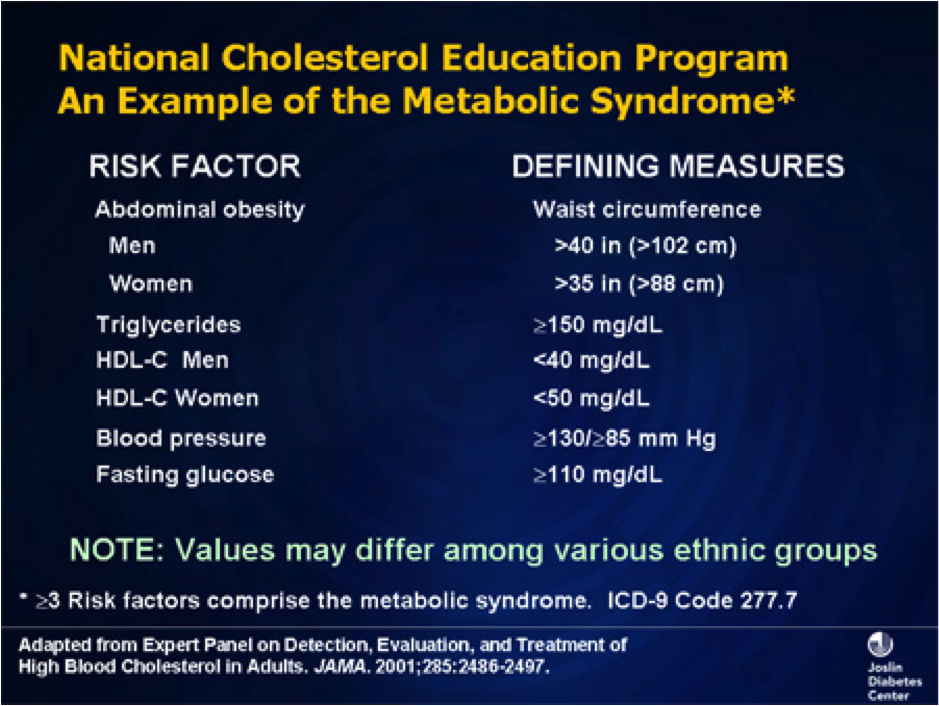
- obesity
- blood pressure ( in some people )
- "vitality"
- mood
- libido
- erections
- muscle strength
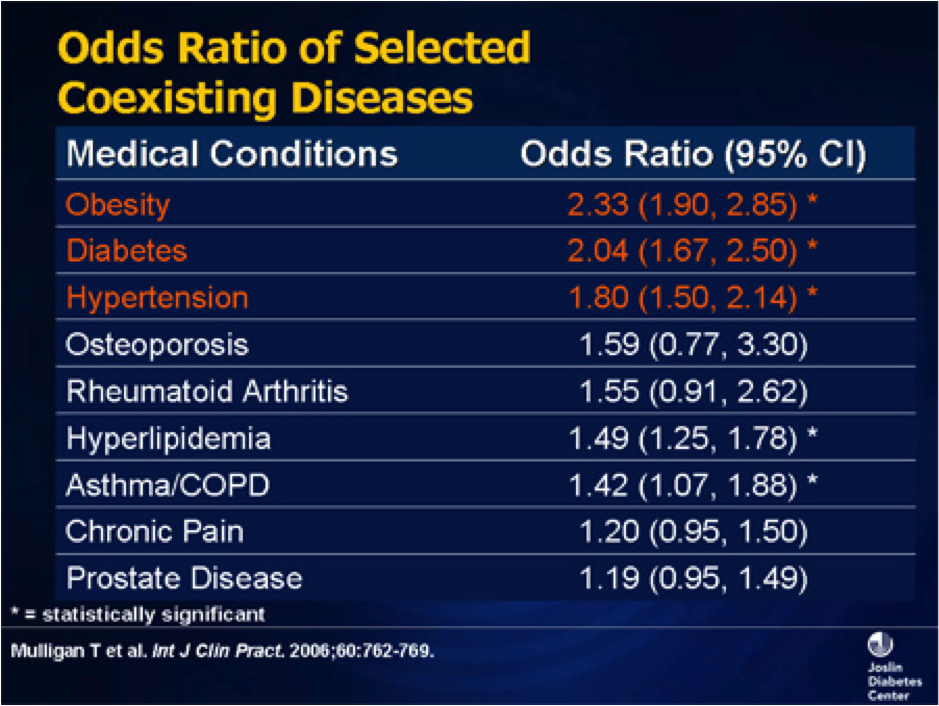
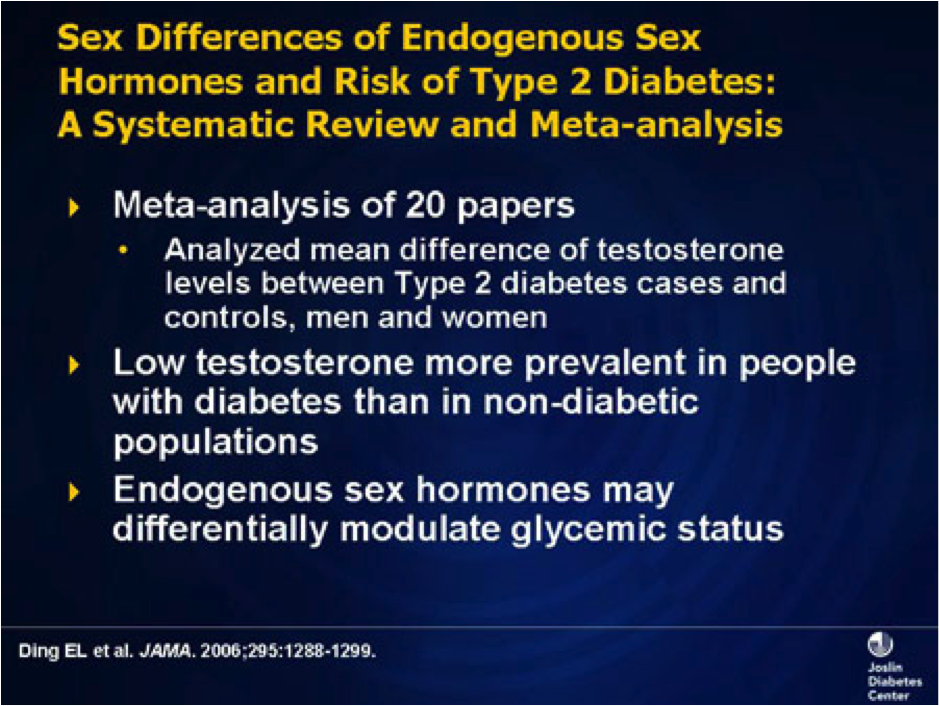
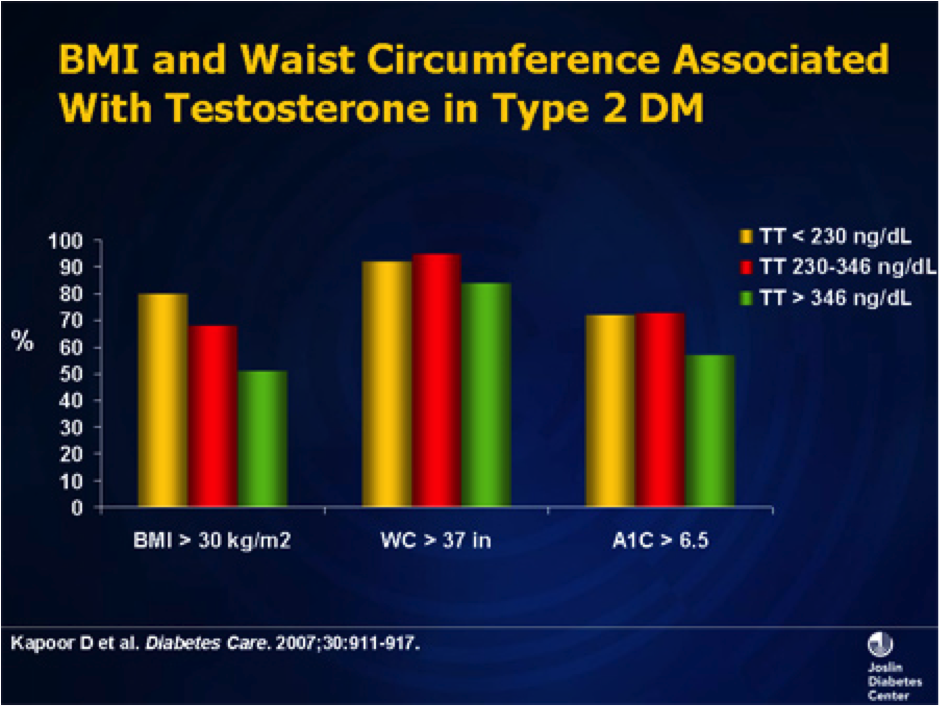
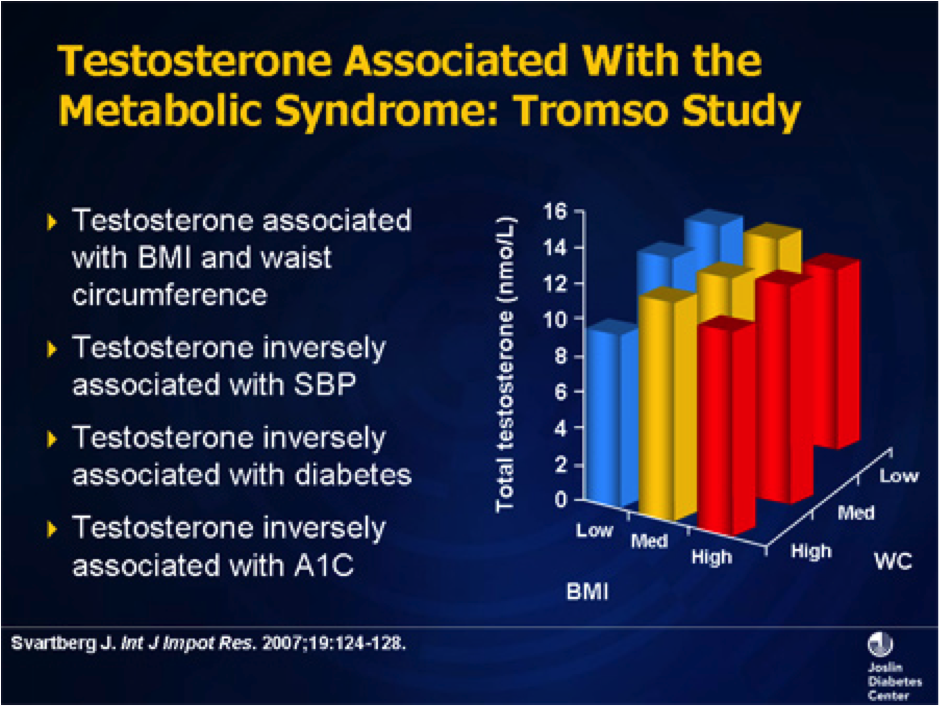
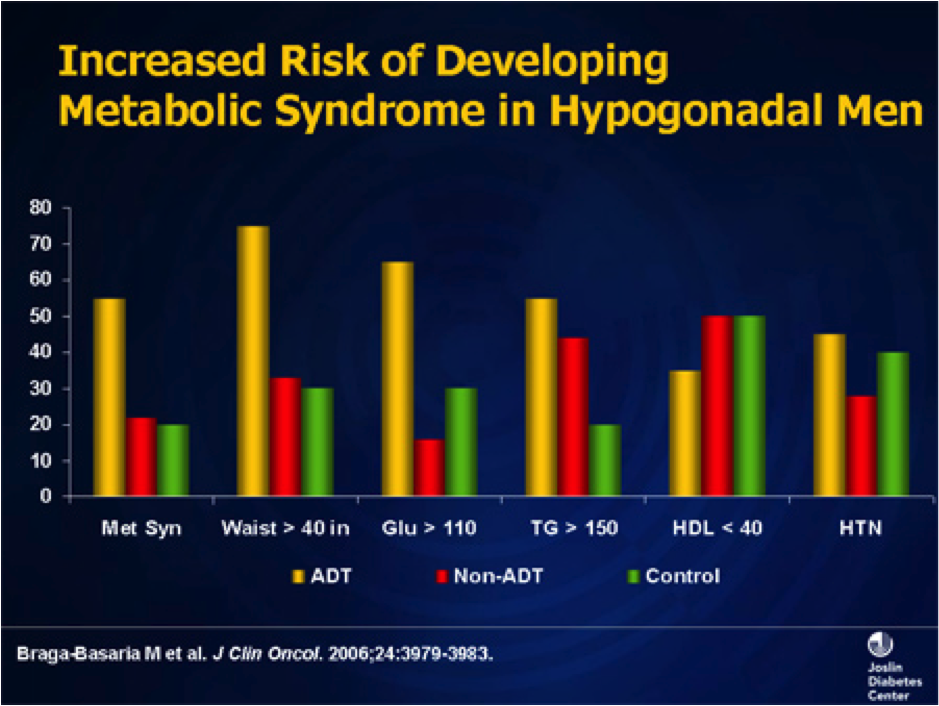
- diabetes
- HIV
- longevity ( take that any way you wish ! )
Testosterone is good for :
- osteoporosis
- anemia
- cholesterol
- heart disease
- obesity
- blood pressure ( in some people )
- "vitality"
- mood
- libido
- erections
- muscle strength
- diabetes
- HIV
- longevity ( take that any way you wish ! )
Testosterone Replacement Therapy (TRT)
- Dr Patrick Nesbitt, Vancouver
- we do a lot of testosterone replacement here at the office. So here is some information about the pros and cons. Bear in mind that doctors seldom agree on things, so for almost every article there is a competing expert who thinks the exact opposite !
NERDY REFERENCE ARTICLES
Not treating low T may cause prostate cancer
Testosterone and sexual function
How to increase your T level naturally
Testosterone gels may be safer than the injections
No cardiovascular risk seen in latest testosterone study
Summary of Canadian Journal of Urology about TRT
Testosterone Improves Sexual Function in Men Across the Board
Testosterone Levels and Survival in Diabetic Men
Testosterone may increase risk of blood clots, especially 1rst 6 months
Most recent NIH Trial about risks/benefits of TRT
Boner pills and testosterone may help diabetic men live longer
Vitamin D may improve low testosterone levels
Controversies re cardiac effects of testosterone replacement
Clomipne and hCG
Controversies about what is a normal T level for a young man
Testosterone levels are declining
Treating " aging" with Testosterone
In Men over 70 "Free T" may be the thing to check
How do I know if I am low on Testosterone ?
There are a variety of questionnaires which can help diagnose low T.
The one shown below is called ADAM ( Androgren Deficiency in Aging Male)
1. Do you have a decrease in libido (sex drive)? Yes No
2. Do you have a lack of energy? Yes No
3. Do you have a decrease in strength and/or endurance? Yes No
4. Have you lost height? Yes No
5. Have you noticed a decreased "enjoyment of life" Yes No
6. Are you sad and/or grumpy? Yes No
7. Are your erections less strong? Yes No
8. Have you noticed a recent deterioration in your ability to play sports? Yes No
9. Are you falling asleep after dinner? Yes No
10. Has there been a recent deterioration in your work performance? Yes No
If you Answer Yes to number 1 or 7 or if you have a "yes" to any three answers, then you may be low on testosterone
The one shown below is called ADAM ( Androgren Deficiency in Aging Male)
1. Do you have a decrease in libido (sex drive)? Yes No
2. Do you have a lack of energy? Yes No
3. Do you have a decrease in strength and/or endurance? Yes No
4. Have you lost height? Yes No
5. Have you noticed a decreased "enjoyment of life" Yes No
6. Are you sad and/or grumpy? Yes No
7. Are your erections less strong? Yes No
8. Have you noticed a recent deterioration in your ability to play sports? Yes No
9. Are you falling asleep after dinner? Yes No
10. Has there been a recent deterioration in your work performance? Yes No
If you Answer Yes to number 1 or 7 or if you have a "yes" to any three answers, then you may be low on testosterone
Testosterone nomogram
Educational Videos

Click on here to see a JAMA lecture on Testosterone Replacement
(Also a wee bit dated, but very official and correct - both ways. )
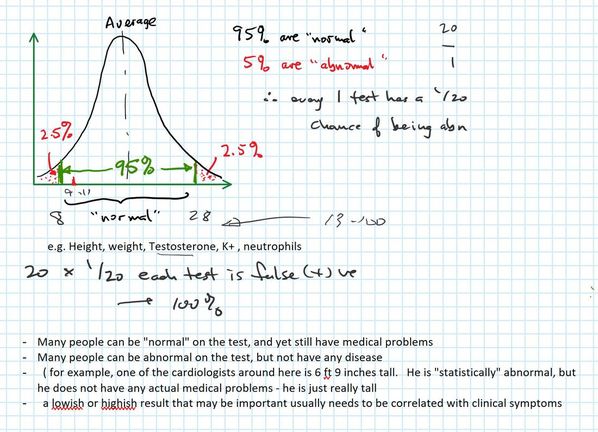
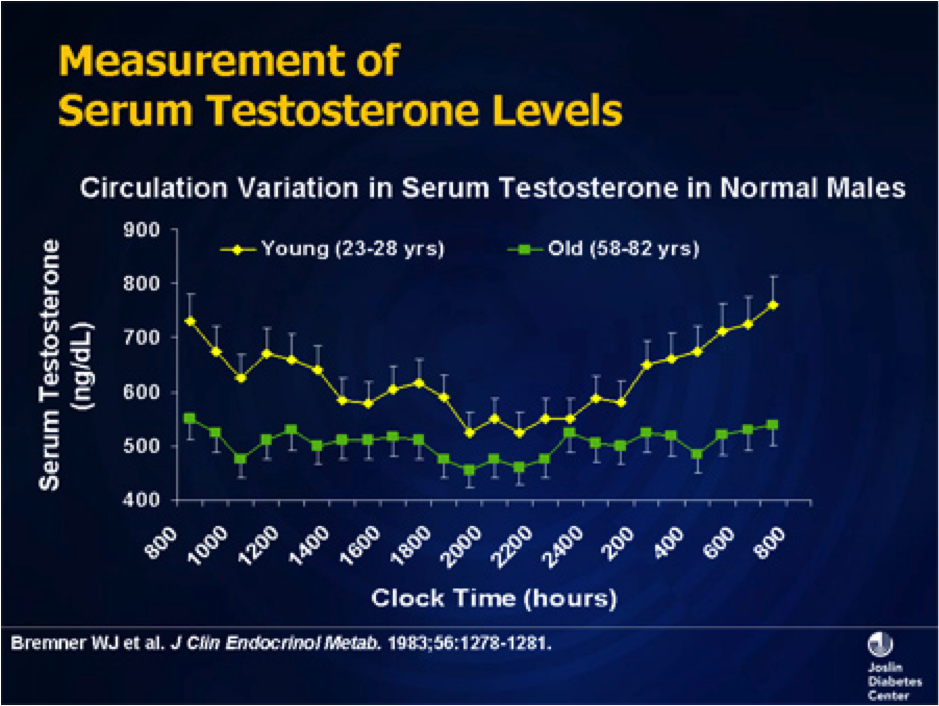
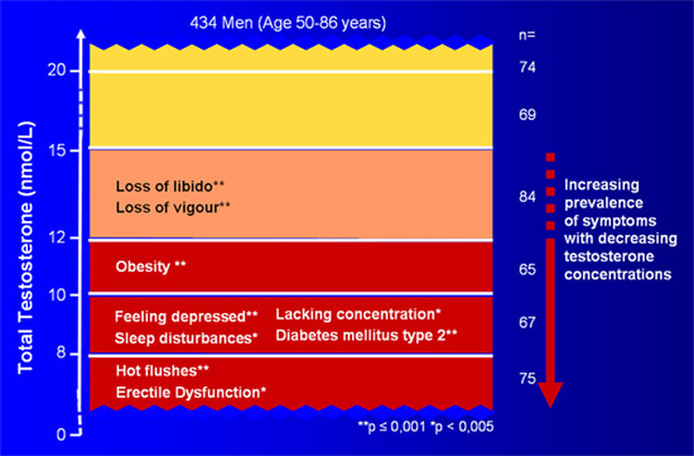
What are normal age related T levels ?

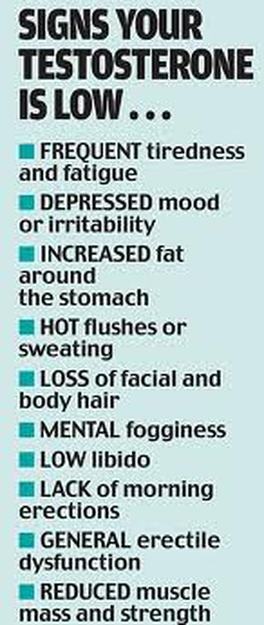
This is a bit of a trick question. T levels get lower as a man gets older. But T levels seem to be declining generally as well.
For example, a 45 year old man will have a higher T level than a 65 year old man.
But a 45 year old man from 2000 would have a higher T level than a 45 year old man from 2017.
So testosterone levels are like the arctic ice - both are slowing disappearing !
Also, to "officially" have a low T you have to be in the lowest 3% of the population for T. But many people have symptoms without being officially low ...
For example, a 45 year old man will have a higher T level than a 65 year old man.
But a 45 year old man from 2000 would have a higher T level than a 45 year old man from 2017.
So testosterone levels are like the arctic ice - both are slowing disappearing !
Also, to "officially" have a low T you have to be in the lowest 3% of the population for T. But many people have symptoms without being officially low ...
Testosterone Replacement Therapy (TRT)

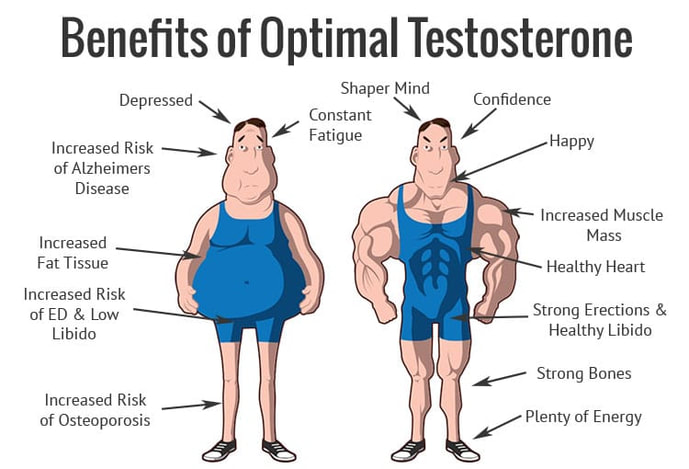
The goal of TRT is not to make anyone into a muscle-bound hulk or a studmuffin.
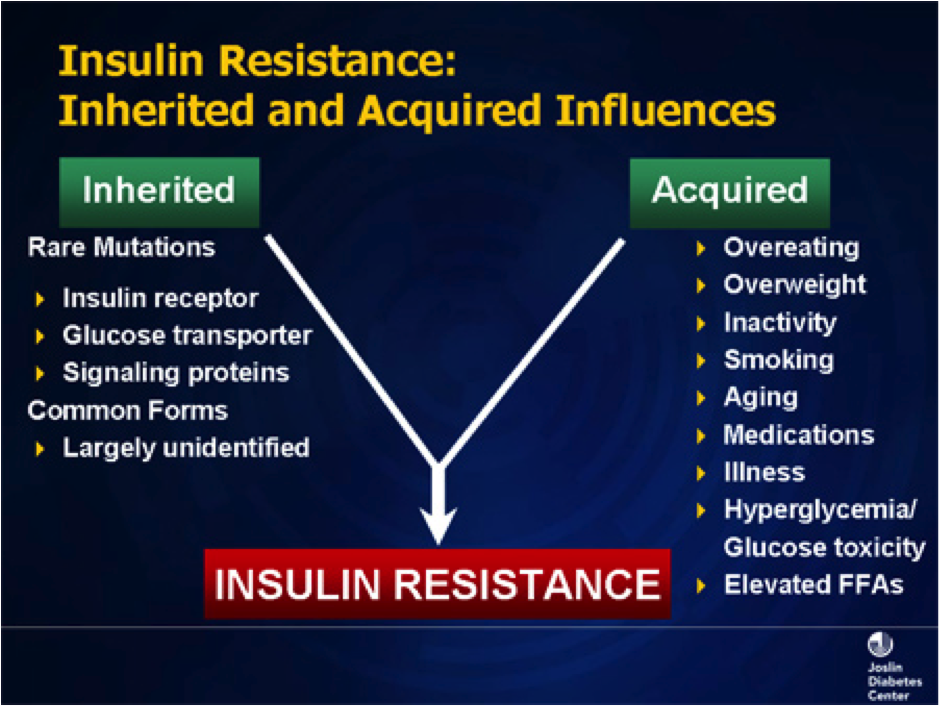
However, mental or physical stressors ( such as heart disease, diabetes, or cancer ) throw your natural hormone levels out of whack, and testosterone is suppressed.
Or sometimes it just happen with natural aging.
Restoring testosterone to normal physiological levels is then good for overall health. Men with high testosterone levels live longer, have less heart disease, better cholesterol, stronger bones, and more vitality.
And it also can increase your libido and erections. Which - if you are in the age group where medically approved testosterone is indicated - can either be wonderful, or a huge nuisance to your wife !
It is also completely recommended by medical experts and mainstream medicine. With certain precautions, which you can read about below.
However, mental or physical stressors ( such as heart disease, diabetes, or cancer ) throw your natural hormone levels out of whack, and testosterone is suppressed.
Or sometimes it just happen with natural aging.
Restoring testosterone to normal physiological levels is then good for overall health. Men with high testosterone levels live longer, have less heart disease, better cholesterol, stronger bones, and more vitality.
And it also can increase your libido and erections. Which - if you are in the age group where medically approved testosterone is indicated - can either be wonderful, or a huge nuisance to your wife !
It is also completely recommended by medical experts and mainstream medicine. With certain precautions, which you can read about below.
The Bad
There are only two really possible bad things about TRT, and they are both still somewhat disputed.
1) Does TRT cause an increase in prostate cancer?
A: No !!! ( It actually probably decreases prostate cancer )
2) Is Testosterone bad for your heart, neutral, or good for your heart ?
A: Probably good, but no one knows for sure
irst we thought that testosterone was bad for your heart. Then we thought it was good for your heart. Then, in a JAMA article - the 3rd most reputable journal in the world ( after NEJM and Lancet ) they said it was bad again. ( This article and an editorial about it can be found at the very bottom of this page. ) And now pretty much everyone thinks the JAMA article is totally stupid and useless.
Testosterone can :
- increase libido
- slightly increase male breast cancer
( incidence 1/700)
- thicken your blood
( although mostly only if injected) - this could theoretically incr. chances of blood clots, but no one is sure yet whether or not this really happens )
- shrink your testicles ( a tiny bit )
- make it harder to get women pregnant ( but there is a way around that for those who are interested. )
Testosterone can :
- increase libido
- slightly increase male breast cancer
( incidence 1/700)
- thicken your blood
( although mostly only if injected) - this could theoretically incr. chances of blood clots, but no one is sure yet whether or not this really happens )
- shrink your testicles ( a tiny bit )
- make it harder to get women pregnant ( but there is a way around that for those who are interested. )
More about the bad - TRT, Prostate Cancer and Heart Attacks
1 ) Prostate Cancer:
We used to think that testosterone increased prostate cancer. "Pouring flames on the fire" was the usual description. Now we know that high testosterone seems to protect against prostate cancer.
Currently we go for a "saturation of receptors" model. Think of the prostate as a dishwashing sponge. If you are testosterone depleted your sponge will get dried up and shrunken. If you replace the missing testosterone, the sponge returns to it's normal size. If you add even more testosterone what happens to the sponge is ...... nothing ! ( A sponge can only get as big as a sponge can get. )
So if you are low in testosterone and get TRT your prostate may enlarge a bit at the beginning. But only back to the size it would have been under conditions of a normal amount of testosterone. And no more.
TESTOSTERONE DOES NOT CAUSE AN INCREASE IN PROSTATE CANCER
1 ) Prostate Cancer:
We used to think that testosterone increased prostate cancer. "Pouring flames on the fire" was the usual description. Now we know that high testosterone seems to protect against prostate cancer.
Currently we go for a "saturation of receptors" model. Think of the prostate as a dishwashing sponge. If you are testosterone depleted your sponge will get dried up and shrunken. If you replace the missing testosterone, the sponge returns to it's normal size. If you add even more testosterone what happens to the sponge is ...... nothing ! ( A sponge can only get as big as a sponge can get. )
So if you are low in testosterone and get TRT your prostate may enlarge a bit at the beginning. But only back to the size it would have been under conditions of a normal amount of testosterone. And no more.
TESTOSTERONE DOES NOT CAUSE AN INCREASE IN PROSTATE CANCER
Testosterone AFTER prostate cancer.
Yes, that is a possibility! If you have had prostate cancer and have had it treated , then your love life may be less than it was. And you can - if you are an appropriate candidate - have TRT even after prostate cancer. The main qualifications are :
a) The cancer has to have been confined to the prostate
b) Two years after the surgery or radiation your PSA levels must still be undetectable.
If the above two conditions are met, you may be a candidate for testosterone replacement therapy - even post prostate cancer .
Yes, that is a possibility! If you have had prostate cancer and have had it treated , then your love life may be less than it was. And you can - if you are an appropriate candidate - have TRT even after prostate cancer. The main qualifications are :
a) The cancer has to have been confined to the prostate
b) Two years after the surgery or radiation your PSA levels must still be undetectable.
If the above two conditions are met, you may be a candidate for testosterone replacement therapy - even post prostate cancer .
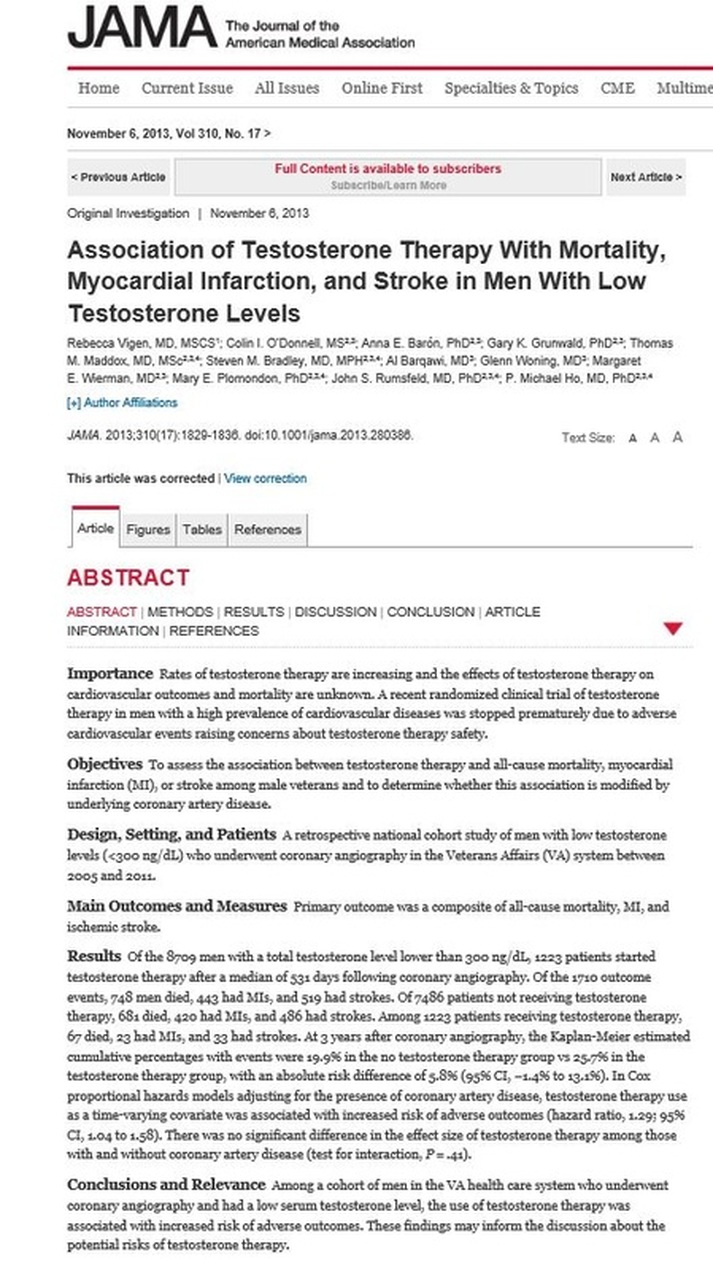
Testosterone and the Heart - Much Ado About crap !
The article at the left can be found further down at the very very bottom of this page. Where is deserves to be. It says that testosterone replacement increases heart attack risk. However, this study has made almost every error it is possible to make in a scientific study.
The cries for it to be recalled began only four days after it's initial publication. It has now been criticised by 29 medical societies in 32 countries. It has been criticized in every continent but Antarctica. It was such a bad study in every way that one of the editors of JAMA got fired for publishing it.
The article at the left can be found further down at the very very bottom of this page. Where is deserves to be. It says that testosterone replacement increases heart attack risk. However, this study has made almost every error it is possible to make in a scientific study.
The cries for it to be recalled began only four days after it's initial publication. It has now been criticised by 29 medical societies in 32 countries. It has been criticized in every continent but Antarctica. It was such a bad study in every way that one of the editors of JAMA got fired for publishing it.
The Truly Evil JAMA Testosterone Study
This study was done from "data dredging " of a bunch of databases from VA ( Veterans Administration ) hospitals in the U.S.
It was not the result of a considered experiment. It was the hindsight product of a bunch of clueless computer nerds who went sifting through databases looking for correlations. In a particularly imcompetent manner.
This study was done from "data dredging " of a bunch of databases from VA ( Veterans Administration ) hospitals in the U.S.
It was not the result of a considered experiment. It was the hindsight product of a bunch of clueless computer nerds who went sifting through databases looking for correlations. In a particularly imcompetent manner.
The Ugly
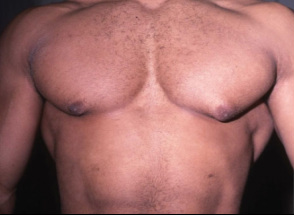
Testosterone can :
- cause 'man boobs' / gynecomastia/ bitch tits ( although mainly the types of T abused by body builders)
- accelerate male pattern baldness ( although there is an antidote, which actually is actually good for getting even more hair, and prevents prostate cancer. )
- Shrink your testicles ( click here for an explanation why )
- cause 'man boobs' / gynecomastia/ bitch tits ( although mainly the types of T abused by body builders)
- accelerate male pattern baldness ( although there is an antidote, which actually is actually good for getting even more hair, and prevents prostate cancer. )
- Shrink your testicles ( click here for an explanation why )
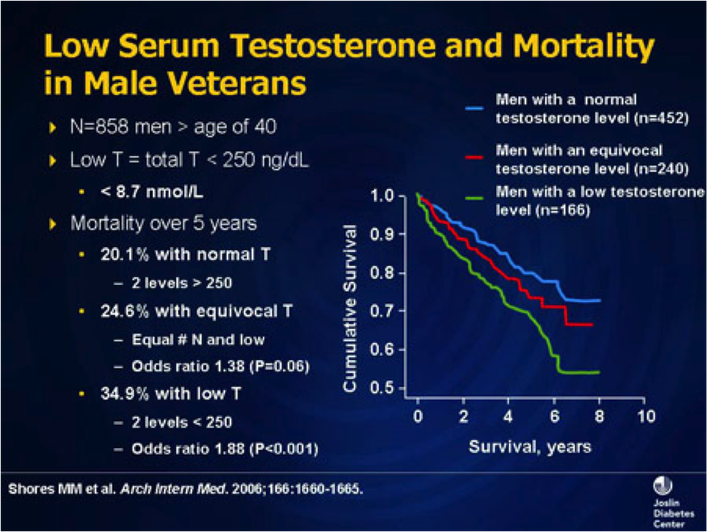
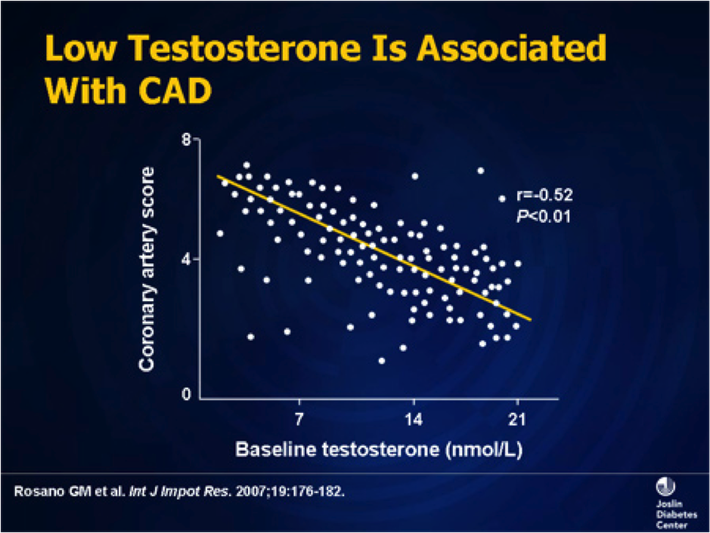
Testosterone makes men live longer !

My apologies for the boring slides below. Part of the reason I am including some of them is to show that testosterone replacement is a lot like regular medicine - complicated, scientific, and fascinating in it's potential, but boring in the details. ( Except to us nerds.)
The slides below show that as testosterone levels go up ( the horizontal axis ) , Coronary Artery Disease, or CAD goes down. Which shows that testosterone is good for your heart. Low testosterone means more heart attacks. Normal testosterone means less heart attacks.
And the slide after that shows that the higher your testosterone the longer you live !
Which illustrates a critical concept - testosterone is good for body parts other than just your penis !!!
The slides below show that as testosterone levels go up ( the horizontal axis ) , Coronary Artery Disease, or CAD goes down. Which shows that testosterone is good for your heart. Low testosterone means more heart attacks. Normal testosterone means less heart attacks.
And the slide after that shows that the higher your testosterone the longer you live !
Which illustrates a critical concept - testosterone is good for body parts other than just your penis !!!
Testosterone helps moody morose old men ...
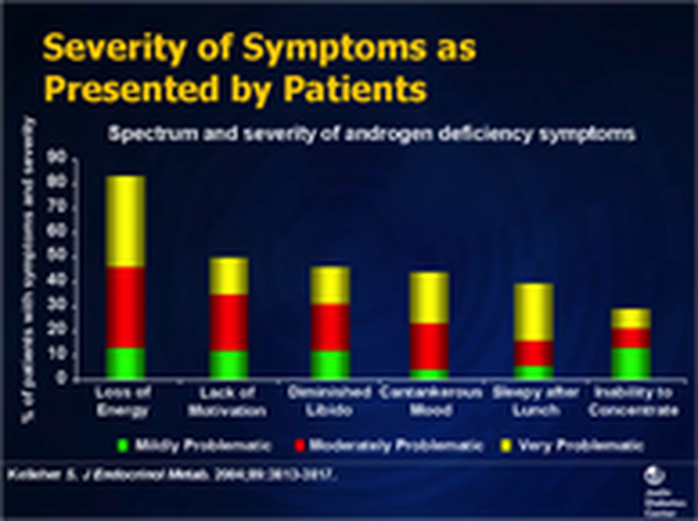
Testosterone stimulates the brain in a positive way. This graph shows some of the positive mental changes that come from having healthy Testosterone levels.
What happens as T levels fall .
.
Is Testosterone Replacement Controversial ?
Yup!
Testosterone replacement is like a lot of medical conditions. We know some of the answers, but not all of them. So some things are generally agreed on, and some are debated. Such is life !
If you are low on testosterone, then testosterone replacement is generally a "good thing".
If you are taking testosterone to give yourself huge muscles or turn yourself into a sex machine, then you are either an idiot or a young man. The two conditions often co-exist !
Incidentally, the bigger the muscles, the smaller the testicles. ( Check it out ladies !)
Testosterone replacement is like a lot of medical conditions. We know some of the answers, but not all of them. So some things are generally agreed on, and some are debated. Such is life !
If you are low on testosterone, then testosterone replacement is generally a "good thing".
If you are taking testosterone to give yourself huge muscles or turn yourself into a sex machine, then you are either an idiot or a young man. The two conditions often co-exist !
Incidentally, the bigger the muscles, the smaller the testicles. ( Check it out ladies !)
There are really only two reasons why testosterone replacement appears controversial :
1) Young men might want to abuse testosterone
- there was once a study where 18 year old men were asked whether or not they would take steroids if they could be muscle bound sex monsters till their thirtieth birthday, upon which they would die. The majority said yes. Because they were young, stupid, and could not imagine ever getting as old as thirty !
2) There are sooooo many old men who might benefit from testosterone that health plans are reluctant to acknowledge it. It could get expensive !
- some medical experts feel that 40 % of men over the age of 45 are low on testosterone and could benefit from testosterone replacement. Hence all the ads on American TV asking " have you got low T ? ". Americans love a good market ! And Canadian health care plans are trying to save money. So some people are trying to promote testosterone, and others are trying to restrict it.
1) Young men might want to abuse testosterone
- there was once a study where 18 year old men were asked whether or not they would take steroids if they could be muscle bound sex monsters till their thirtieth birthday, upon which they would die. The majority said yes. Because they were young, stupid, and could not imagine ever getting as old as thirty !
2) There are sooooo many old men who might benefit from testosterone that health plans are reluctant to acknowledge it. It could get expensive !
- some medical experts feel that 40 % of men over the age of 45 are low on testosterone and could benefit from testosterone replacement. Hence all the ads on American TV asking " have you got low T ? ". Americans love a good market ! And Canadian health care plans are trying to save money. So some people are trying to promote testosterone, and others are trying to restrict it.
.
Testosterone levels are falling in men over the generations :
These graphs below show that for some reason male testosterone levels have been decreasing over time. No one knows exactly why, but it is a fact. And I have a few theories as to why :
a) Wimslib - don' ask me why, but testosterone seems to be unfashionable these days. ( Except for MMA fans. )
b) Microwaves
c) TV dinners
I think the last two may be related.
TV dinners are incased in a synthetic plastic trays which - when exposed to microwaves - leech small amounts of chemicals into the food. These chemicals have testosterone-opposing activity.
Countries that have more microwave ovens and more TV dinners are the same countries that have declining testosterone levels. And declining sperm counts as well. Sure it is a goofy theory. But what if I am correct ?
These graphs below show that for some reason male testosterone levels have been decreasing over time. No one knows exactly why, but it is a fact. And I have a few theories as to why :
a) Wimslib - don' ask me why, but testosterone seems to be unfashionable these days. ( Except for MMA fans. )
b) Microwaves
c) TV dinners
I think the last two may be related.
TV dinners are incased in a synthetic plastic trays which - when exposed to microwaves - leech small amounts of chemicals into the food. These chemicals have testosterone-opposing activity.
Countries that have more microwave ovens and more TV dinners are the same countries that have declining testosterone levels. And declining sperm counts as well. Sure it is a goofy theory. But what if I am correct ?
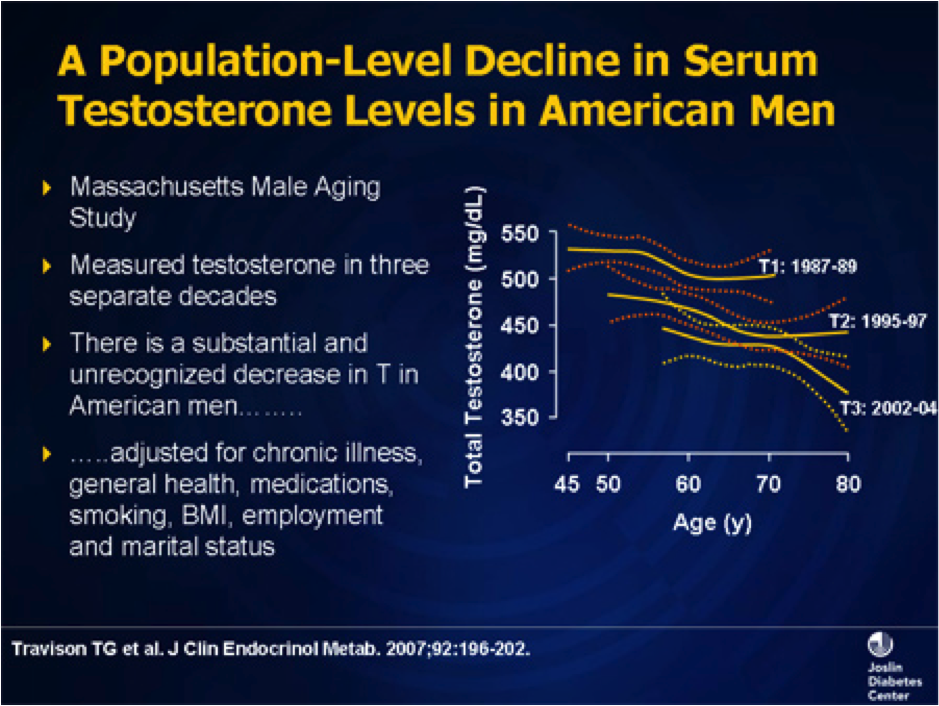
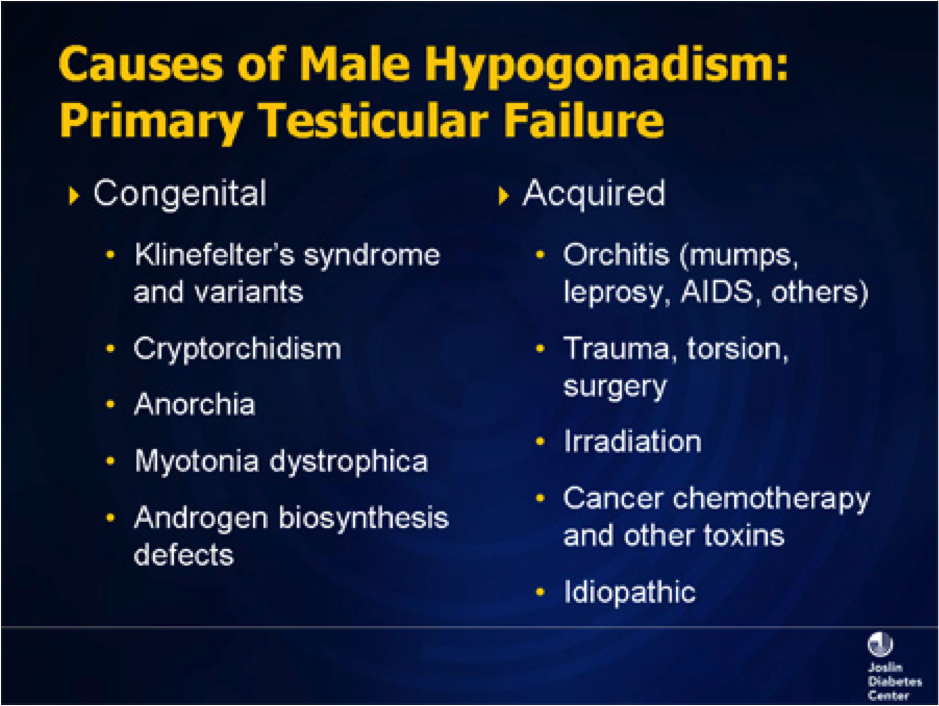
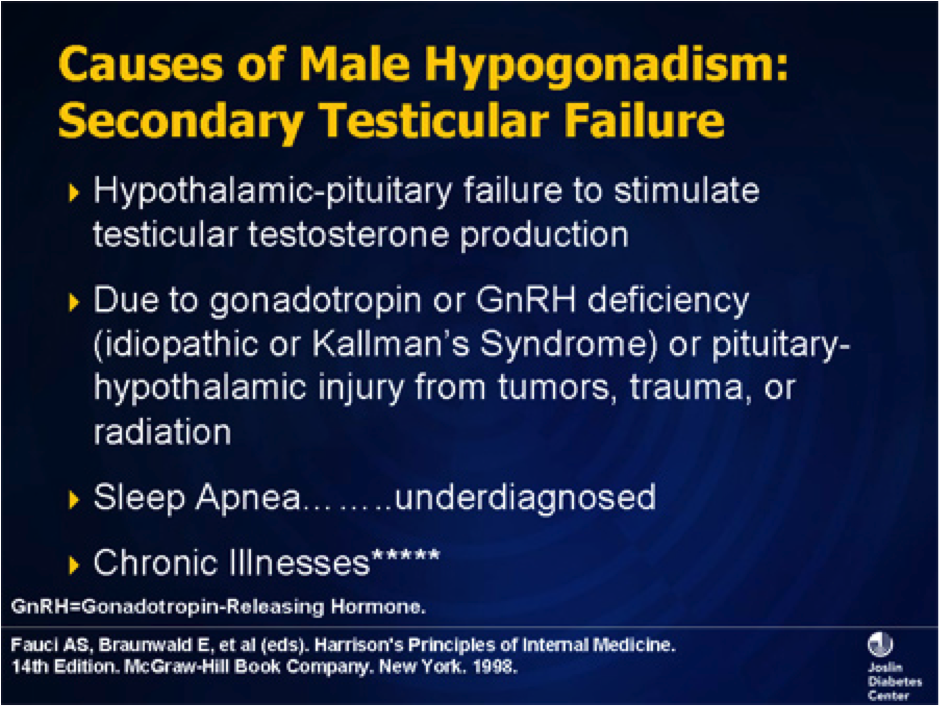
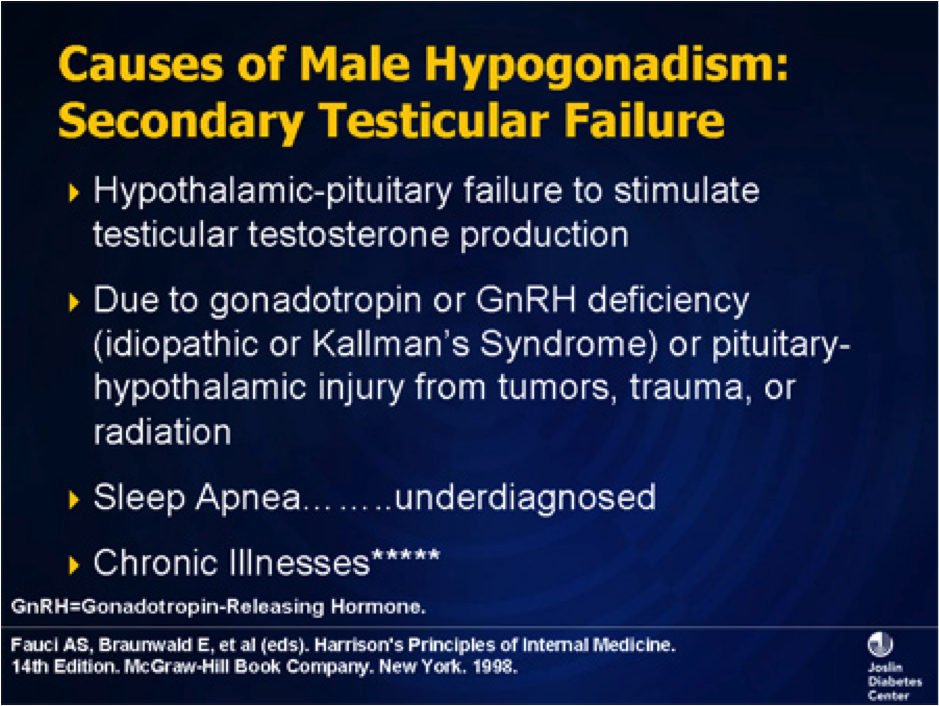
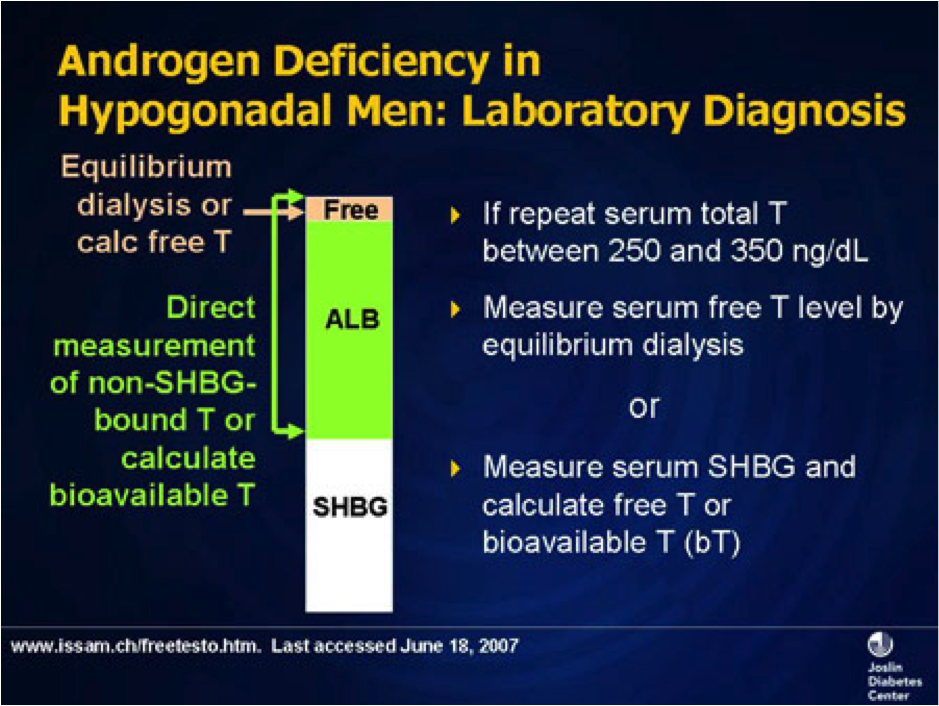
This is where testosterone comes from and how we measure it.
The pituitary gland is the master gland of the body. It produces two hormones
1) FSH - "Follicle Stimulating Hormone". Dumb name, and it has nothing to do with anything, but this is the hormone that stimulates production of testosterone and sperm.
2) LH - "Luteinizing Hormone." Another dumb name. But this is the hormone that makes testosterone.
The pituitary gland is the master gland of the body. It produces two hormones
1) FSH - "Follicle Stimulating Hormone". Dumb name, and it has nothing to do with anything, but this is the hormone that stimulates production of testosterone and sperm.
2) LH - "Luteinizing Hormone." Another dumb name. But this is the hormone that makes testosterone.
These are some of the symptoms of being low and Testosterone. And here you thought you just liked an afternoon nap ! But lack of libido, low motivation, and falling aslepp after lunch can all be signs of low Testosterone. ( Or Obstructive Sleep Apnea - if you snore, you should get checked for this as well. But that is another subject !)
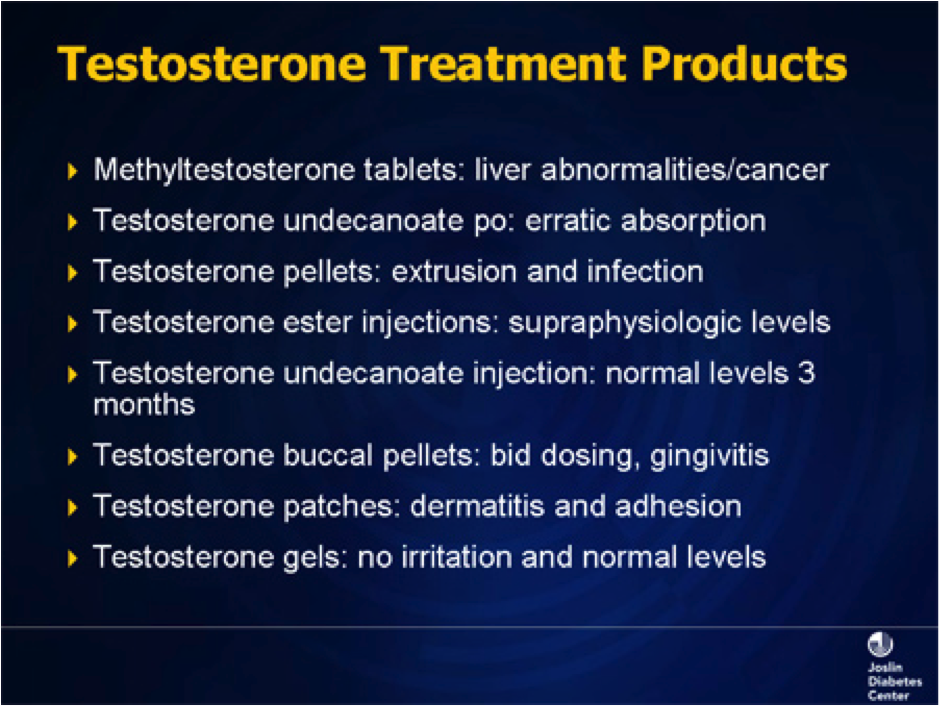
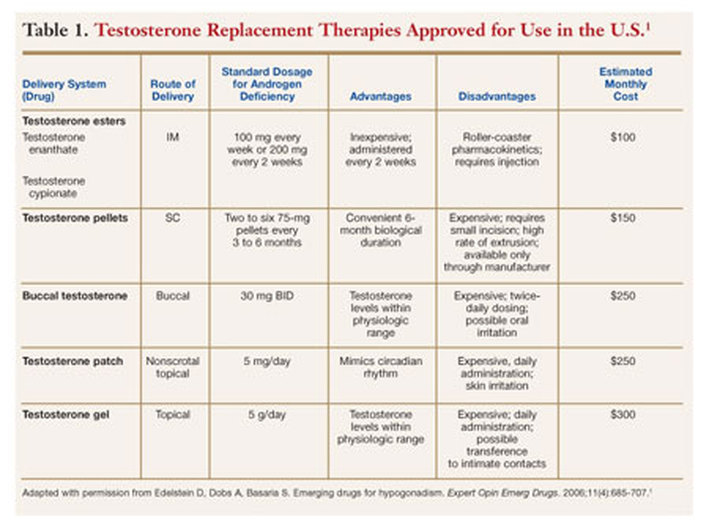
For some reason this slide doesn't mention testosterone pills.
These are available in Canada , and are meant to be taken twice a day.
Unfortunately, to be absorbed properly they should be eaten with a fatty meal twice a day.
Not a good idea for men taking testosterone for heart health reasons !
These are available in Canada , and are meant to be taken twice a day.
Unfortunately, to be absorbed properly they should be eaten with a fatty meal twice a day.
Not a good idea for men taking testosterone for heart health reasons !
Testosterone Replacement Medical Articles 2012
Below are a bunch of boring articles pasted directly from medical journals.
They are not so much for lay people to read and understand as just to convince you that I am not kidding about all of the stuff I said above about testosterone replacement.
J Clin Endocrinol Metab. 2012 Jun;97(6):2050-8. Epub 2012 Apr 11.
Testosterone treatment and mortality in men with low testosterone levels.
Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM.
Source
Veterans Affairs Puget Sound Health Care System, 1660 South Columbian Way, S-116PES, Seattle, Washington 98108, USA. [email protected]
Abstract
CONTEXT:
Low testosterone levels in men have been associated with increased mortality. However, the influence of testosterone treatment on mortality in men with low testosterone levels is not known.
OBJECTIVE:
The objective of the study was to examine the association between testosterone treatment and mortality in men with low testosterone levels.
DESIGN:
This was an observational study of mortality in testosterone-treated compared with untreated men, assessed with time-varying, adjusted Cox proportional hazards regression models. Effect modification by age, diabetes, and coronary heart disease was tested a priori.
SETTING:
The study was conducted with a clinical database that included seven Northwest Veterans Affairs medical centers.
PATIENTS:
Patients included a cohort of 1031 male veterans, aged older than 40 yr, with low total testosterone [≤250 ng/dl (8.7 nmol/liter)] and no history of prostate cancer, assessed between January 2001 and December 2002 and followed up through the end of 2005.
MAIN OUTCOME MEASURE:
Total mortality in testosterone-treated compared with untreated men was measured.
RESULTS:
Testosterone treatment was initiated in 398 men (39%) during routine clinical care. The mortality in testosterone-treated men was 10.3% compared with 20.7% in untreated men (P<0.0001) with a mortality rate of 3.4 deaths per 100 person-years for testosterone-treated men and 5.7 deaths per 100 person-years in men not treated with testosterone. After multivariable adjustment including age, body mass index, testosterone level, medical morbidity, diabetes, and coronary heart disease, testosterone treatment was associated with decreased risk of death (hazard ratio 0.61; 95% confidence interval 0.42-0.88; P = 0.008). No significant effect modification was found by age, diabetes, or coronary heart disease.
CONCLUSIONS:
In an observational cohort of men with low testosterone levels, testosterone treatment was associated with decreased mortality compared with no testosterone treatment. These results should be interpreted cautiously because residual confounding may still be a source of bias. Large, randomized clinical trials are needed to better characterize the health effects of testosterone treatment in older men with low testosterone levels.
J Urol. 2012 Apr;187(4):1369-73. Epub 2012 Feb 15.
Performance of total testosterone measurement to predict free testosterone for the biochemical evaluation of male hypogonadism.
Anawalt BD, Hotaling JM, Walsh TJ, Matsumoto AM.
Source
Department of Medicine, University of Washington and Geriatric Research, Seattle, Washington 98195, USA. [email protected]
Abstract
PURPOSE:
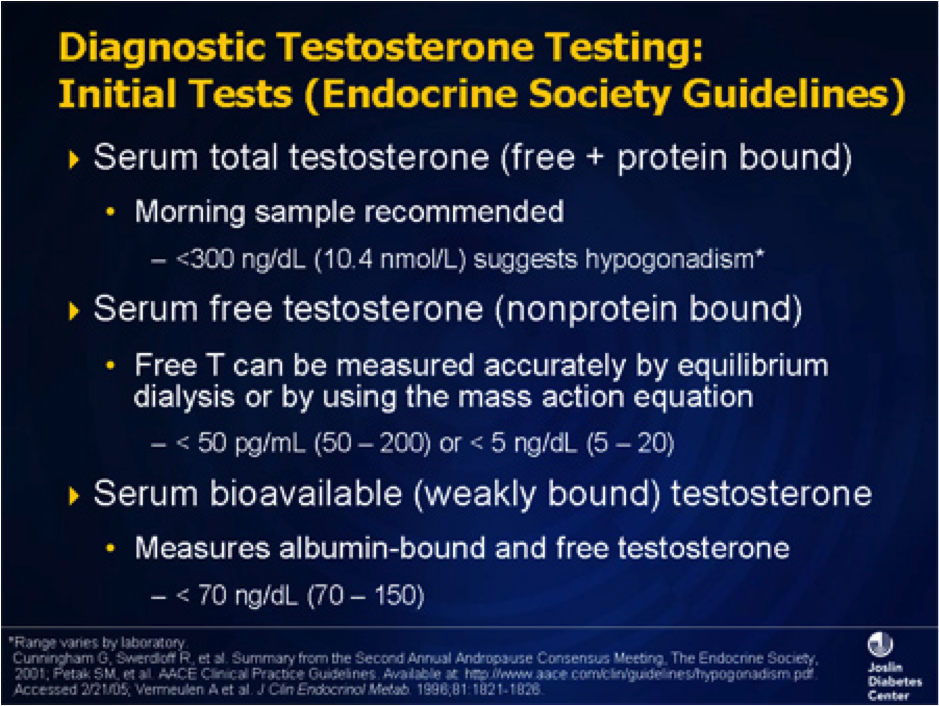
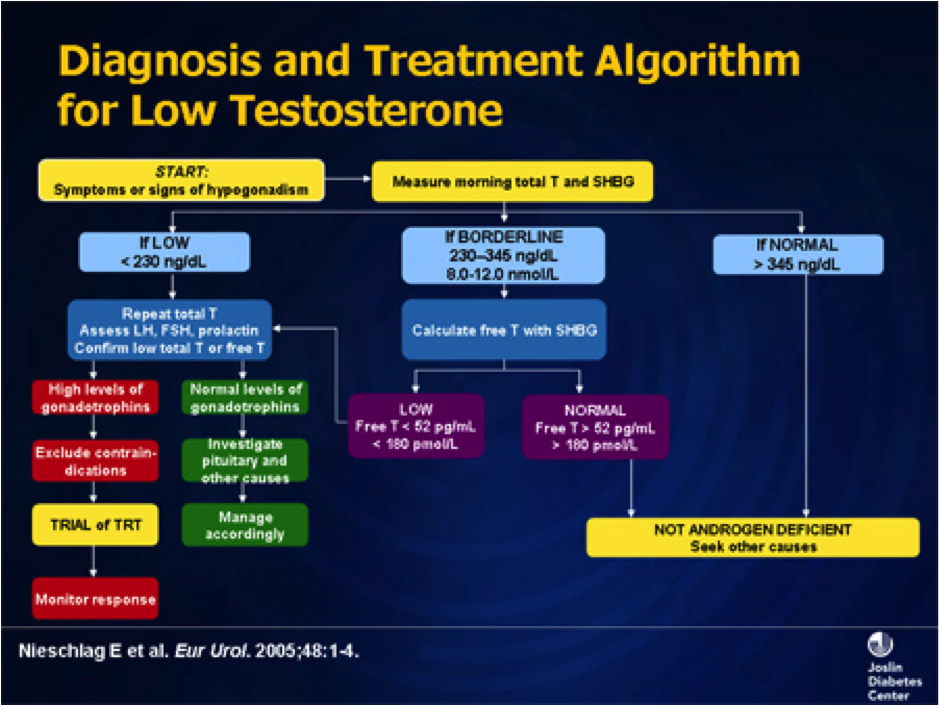
Guidelines recommend serum total testosterone measurement as the initial test to evaluate male hypogonadism, reserving free testosterone assessment for men with suspected sex hormone-binding globulin abnormalities or total testosterone near the lower limit of normal. We determined the performance of total testosterone measurement as a test to identify men with normal vs low free testosterone.
MATERIALS AND METHODS:
We examined the electronic medical records of all 3,672 men evaluated for hypogonadism by a serum testosterone panel, including total testosterone, sex hormone-binding globulin, albumin and calculated free testosterone, from January 1, 1997 through December 31, 2007 in a network that serves veterans in Washington.
RESULTS:
The sensitivity and specificity of low total testosterone (less than 280 ng/dl) to rule out and predict low calculated free testosterone was 91.0% and 73.7%, respectively. At thresholds of less than 350 and less than 400 ng/dl the sensitivity of total testosterone for low calculated free testosterone increased to 96.8% and 98.2%, and at thresholds of less than 150 and less than 200 ng/dl specificity increased to 98.9% and 92.6%, respectively.
CONCLUSIONS:
Total testosterone between 280 and 350 ng/dl is not sensitive enough to reliably exclude hypogonadism. Total testosterone must exceed 350 to 400 ng/dl to reliably predict normal free testosterone. Except when levels are less than 150 ng/dl total testosterone measurement has low specificity for the biochemical diagnosis of hypogonadism.
J Clin Endocrinol Metab. 2012 Aug;97(8):2809-17. Epub 2012 Jun 1.
Impact of male hormonal contraception on prostate androgens and androgen action in healthy men: a randomized, controlled trial.
Mostaghel EA, Lin DW, Amory JK, Wright JL, Marck BT, Nelson PS, Matsumoto AM, Bremner WJ, Page ST.
Source
AssociateDivision of Metabolism, Endocrinology, and Nutrition, University of Washington School of Medicine, Box 357138, 1959 NE Pacific Street, Seattle, Washington 98195. [email protected].
Abstract
Context: Male hormonal contraception (MHC) combines hypothalamic-pituitary-gonadal axis blockade with exogenous androgen delivery to maintain extragonadal androgen end-organ effects. Concern exists that MHC may adversely impact prostate health. Objective: The objective of the study was to determine the molecular impact of MHC on intraprostatic androgen concentrations and androgen action. Design: This was a single-blind, randomized, placebo-controlled study. Setting: The study was conducted at an academic medical center. Participants: 32 healthy men aged 25-55 yr participated in the study. Intervention: Interventions included placebo, daily transdermal testosterone (T) (T-gel), T-gel + depomedroxyprogesterone acetate (T+DMPA), or T-gel + dutasteride daily (T+D) for 12 wk, and prostate biopsy during treatment wk 10. Main Outcome Measures: Serum and prostate androgen concentrations and prostate epithelial-cell gene expression were measured. Results: Thirty men completed the study. Serum T levels were significantly increased in T-gel and T+D groups compared with baseline (P < 0.05) but were decreased with the addition of DMPA. Intraprostatic androgens were no different from placebo with T-gel treatment. Addition of DMPA to T resulted in 40% lower intraprostatic dihydrotestosterone (DHT) concentration (P = 0.0273 vs. placebo), whereas combining dutasteride with T resulted in a 90% decrease in intraprostatic DHT (P = 0.0012), 11-fold increased intraprostatic T (P = 0.0011), and 7-fold increased intraprostatic androstenedione (P = 0.0011). Significant differences in global or androgen-regulated prostate epithelial-cell gene expression were not observed. Androgen-regulated gene expression correlated with epithelial-cell androgen receptor and prostatic DHT in placebo, T-gel, and T+DMPA arms and with T and androstenedione levels in the T+D arm. Conclusions: MHC regimens do not markedly alter gene expression in benign prostate epithelium, suggesting they may not alter risk of prostate disease. Longer-term studies examining the impact of MHC on prostate health are needed.
J Urol. 2011 Feb;185(2):626-32. Epub 2010 Dec 18.
Oral testosterone with and without concomitant inhibition of 5α-reductase by dutasteride in hypogonadal men for 28 days.
Amory JK, Bush MA, Zhi H, Caricofe RB, Matsumoto AM, Swerdloff RS, Wang C, Clark RV.
Source
University of Washington, Seattle, Washington, USA.
Abstract
PURPOSE:
Co-administration of the 5α-reductase inhibitor dutasteride increases the oral testosterone bioavailability in men with experimentally induced hypogonadism. We examined oral testosterone with and without dutasteride administration in hypogonadal men for 28 days.
MATERIALS AND METHODS:
We randomly assigned 43 hypogonadal men to twice daily oral doses of 150, 250 or 400 mg testosterone with 0.25 mg dutasteride, 400 mg testosterone alone or 0.25 mg dutasteride alone for 28 days in a multicenter study. Subjects underwent pharmacokinetic profiling of serum hormones on days 1 and 28. A total of 32 men completed all study procedures.
RESULTS:
Serum testosterone increased in all groups on testosterone compared with that in the dutasteride only group. At the 400 mg dose the combination of testosterone and dutasteride resulted in average testosterone concentrations that were 2.7 and 4.6 times higher than in the testosterone only group on days 1 and 28, respectively (p <0.01). On day 28 average testosterone was 20% to 30% lower in all groups on testosterone and dutasteride, and 50% lower in the testosterone only group compared with day 1. Serum dihydrotestosterone was suppressed in all groups on dutasteride and increased in the testosterone only group.
CONCLUSIONS:
Oral testosterone administration resulted in a therapeutic serum testosterone concentration in hypogonadal men. Dutasteride improved the oral bioavailability of testosterone while suppressing dihydrotestosterone. Compared with day 1, testosterone was decreased after 28 days of administration. Additional study is warranted of oral testosterone with dutasteride for testosterone deficiency.
J Clin Endocrinol Metab. 2010 Jun;95(6):2536-59.
Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline.
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, Montori VM; Task Force, Endocrine Society.
Source
Boston University School of Medicine, Boston, Massachusetts 02118, USA.
Abstract
OBJECTIVE:
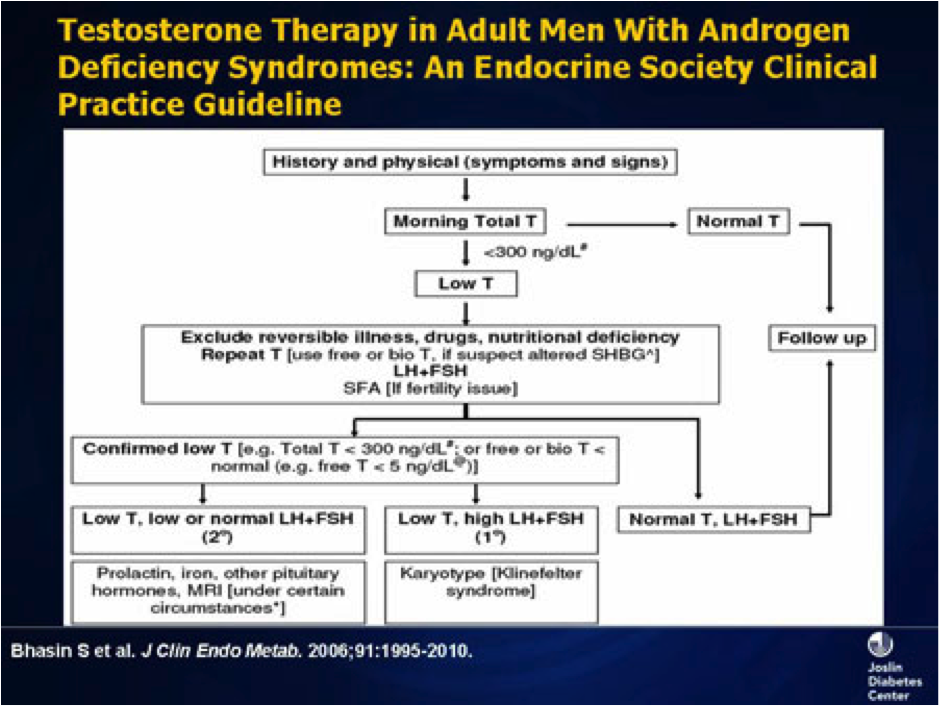
Our objective was to update the guidelines for the evaluation and treatment of androgen deficiency syndromes in adult men published previously in 2006.
PARTICIPANTS:
The Task Force was composed of a chair, selected by the Clinical Guidelines Subcommittee of The Endocrine Society, five additional experts, a methodologist, and a medical writer. The Task Force received no corporate funding or remuneration.
CONCLUSIONS:
We recommend making a diagnosis of androgen deficiency only in men with consistent symptoms and signs and unequivocally low serum testosterone levels. We suggest the measurement of morning total testosterone level by a reliable assay as the initial diagnostic test. We recommend confirmation of the diagnosis by repeating the measurement of morning total testosterone and, in some men in whom total testosterone is near the lower limit of normal or in whom SHBG abnormality is suspected by measurement of free or bioavailable testosterone level, using validated assays. We recommend testosterone therapy for men with symptomatic androgen deficiency to induce and maintain secondary sex characteristics and to improve their sexual function, sense of well-being, muscle mass and strength, and bone mineral density. We recommend against starting testosterone therapy in patients with breast or prostate cancer, a palpable prostate nodule or induration or prostate-specific antigen greater than 4 ng/ml or greater than 3 ng/ml in men at high risk for prostate cancer such as African-Americans or men with first-degree relatives with prostate cancer without further urological evaluation, hematocrit greater than 50%, untreated severe obstructive sleep apnea, severe lower urinary tract symptoms with International Prostate Symptom Score above 19, or uncontrolled or poorly controlled heart failure. When testosterone therapy is instituted, we suggest aiming at achieving testosterone levels during treatment in the mid-normal range with any of the approved formulations, chosen on the basis of the patient's preference, consideration of pharmacokinetics, treatment burden, and cost. Men receiving testosterone therapy should be monitored using a standardized plan.
Endocr J. 2012 Aug 31. [Epub ahead of print]
Increased frequency of anxiety, depression, quality of life and sexual life in young hypogonadotropic hypogonadal males and impacts of testosterone replacement therapy on these conditions.
Aydogan U, Aydogdu A, Akbulut H, Sonmez A, Yuksel S, Basaran Y, Uzun O, Bolu E, Saglam K.
Source
Department of Family Medicine, Gulhane School of Medicine, Ankara 06018, Turkey.
Abstract
Hypogonadotropic hypogonadism is defined as the failure in production of gonadal hormones, thus resulting in lower amounts of testosterone. Depression, anxiety and decreased quality of life are the most common psychopathological conditions in young hypogonadal men. The aim of the present study was to assess the still debated relationship with testosterone levels and psychological symptoms in young male patients with congenital hypogonadotropic hypogonadism (CHH). 39 young male patients with CHH and 40 age-matched healthy males were enrolled in the present study. The impact of testosterone replacement treatment (TRT) on the patients' anxiety and depression levels, sexual function and quality of life were assessed before and after 6 months of treatment using valid and reliable scales, including the Short Form-36 (SF-36), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Arizona Sexual Experiences (ASEX). Patients with CHH had significantly higher scores for BDI, BAI, and ASEX than the control subjects at baseline (p=0.011, p=0.036, p<0.001, respectively). The ASEX and BDI scores significantly improved after the TRT (p<0.001 for both), while the improvement in the BAI score was not statistically significant (p=0.135). When compared to the control group, treatment naïve hypogonadal patients had more severe symptoms of sexual dysfunction, anxiety, depression, and worse quality of life. After 6 months of TRT, we observed improvements in the above parameters, suggesting that low endogenous levels of testosterone might be related to the increased incidence of psychological symptoms.
Metabolism. 2012 Sep 19. pii: S0026-0495(12)00316-2. doi: 10.1016/j.metabol.2012.08.012. [Epub ahead of print]
The complex interaction between obesity, metabolic syndrome and reproductive axis: A narrative review.
Michalakis K, Mintziori G, Kaprara A, Tarlatzis BC, Goulis DG.
Source
First Department of Internal Medicine, Laikon University Hospital, Athens University Medical School, Greece.
Abstract
The aim of this narrative review is to provide current evidence for the interaction between obesity, metabolic syndrome (MS) and reproductive axis. Gonadotropin-releasing hormone (GnRH) pulses and, consequently, normal function of reproductive (hypothalamus-pituitary-gonadal) axis depend on normal energy balance, which presupposes sufficient food intake, reasonable energy consumption and average thermoregulatory costs. In case of an energy imbalance, reproductive dysfunction may occur. In young women, excessive leanness is accompanied by puberty delay, whereas premature puberty might be a manifestation of obesity. In a similar way, obesity in men affects fertility. Excess adipose tissue results in increased conversion of testosterone to estradiol, which may lead to secondary hypogonadism through reproductive axis suppression. Moreover, oxidative stress at the level of the testicular micro-environment may result in decreased spermatogenesis and sperm damage. Products of the adipocyte, such as leptin, adiponectin and resistin, and gut peptides, such as ghrelin, are considered to be crucial in the interaction between energy balance and reproduction. Finally, an indirect evidence for the interplay between MS and reproductive axis is the fact that when treating components of one, parameters of the other can be improved as well. These therapeutic interventions include lifestyle modifications, pharmacological agents, such as sex hormonereplacement therapy, and surgical procedures. Although many issues remain unclear, the elucidation of the complex interaction between MS and reproductive axis will have obvious clinical implications in the therapeutic approach of both entities.
Int J Impot Res. 2012 Sep 13. doi: 10.1038/ijir.2012.29. [Epub ahead of print]
Testosterone replacement therapy in the setting of prostate cancer treated with radiation.
Pastuszak AW, Pearlman AM, Godoy G, Miles BJ, Lipshultz LI, Khera M.
Source
Scott Department of Urology, Baylor College of Medicine, Houston, TX, USA.
Abstract
A lack of consensus and few data support testosterone replacement therapy (TRT) in hypogonadal men who have been treated for prostate cancer (CaP), particularly those who have received radiation therapy. We performed retrospective review of 13 hypogonadal men with CaP, treated with brachytherapy or external beam radiotherapy who were subsequently treated with testosterone (T) between 2006 and 2011. Serum T, free T (FT), estrogen (E), sex hormone-binding globulin (SHBG), prostate-specific antigen (PSA), hemoglobin (Hgb) and hematocrit (Hct) values were evaluated approximately every 3 months after TRT initiation up to 67 months of follow-up. Prostate biopsies demonstrated four men with Gleason (Gl) 6, 7 with Gl 7 and 2 with Gl 8 disease. Median (interquartile range) age at TRT initiation was 68.0 (62.0-77.0) years, initial T 178.0 (88.0-263.5) ng dl(-1), FT 10.1 (5.7-15.0) pg ml(-1) and PSA 0.30 (0.06-0.95) ng ml(-1). Median follow-up after TRT initiation was 29.7 months (range 2.3-67.3 months). At median follow-up, a significant increase in mean T (368.0 (281.3-591.0) ng dl(-1), P=0.012) and SHBG were observed, with no significant increases in Hgb, Hct, E, FT, or PSA (0.66 (0.16-1.35) ng ml(-1), P=0.345). No significant increases in PSA or CaP recurrences were observed at any follow-up interval. TRT in the setting of CaP after treatment with radiation therapy results in a rise in serum T levels and improvement in hypogonadal symptoms without evidence of CaP recurrence or progression.International Journal of Impotence Research advance online publication, 13 September 2012; doi:10.1038/ijir.2012.29.
Clin Interv Aging. 2012;7:321-30. Epub 2012 Aug 24.
Testosterone replacement therapy among elderly males: the Testim Registry in the US (TRiUS).
Bhattacharya RK, Khera M, Blick G, Kushner H, Miner MM.
Source
Department of Internal Medicine, University of Kansas Medical Center, Kansas City, KS, USA;
Abstract
BACKGROUND:
Testosterone levels naturally decline with age in men, often resulting in testosterone deficiency (hypogonadism). However, few studies have examined hypogonadal characteristics and treatment in older (≥65 years) men.
OBJECTIVE:
To compare data at baseline and after 12 months of testosterone replacement therapy (TRT) in hypogonadal men ≥65 vs <65 years old. Data for participants 65-74 vs ≥75 years old were also compared.
METHODS:
Data were from TRiUS (Testim Registry in the United States), which enrolled 849 hypogonadal men treated with Testim(®) 1% (50-100 mg testosterone gel/day) for the first time. Anthropometric, laboratory, and clinical measures were taken at baseline and 12 months, including primary outcomes of total testosterone (TT), free testosterone (FT), and prostate-specific antigen (PSA) levels. Comparisons of parameters were made using Fisher's exact test or analysis of variance. Nonparametric Spearman's ρ and first-order partial correlation coefficients adjusted for the effect of age were used to examine bivariate correlations among parameters.
RESULTS:
Of the registry participants at baseline with available age information, 16% (133/845) were ≥65 years old. They were similar to men <65 years old in the duration of hypogonad-ism prior to enrollment (∼1 year), TT and FT levels at baseline, TT and FT levels at 12-month follow-up, and in reported compliance with treatment. Older patients were more likely to receive lower doses of TRT. PSA levels did not statistically differ between groups after 12 months of TRT (2.18 ± 2.18 ng/mL for ≥65 vs 1.14 ± 0.84 ng/mL for <65 years old, P = 0.1). Baseline values for the >75-year-old subcohort were not significantly different from subcohorts aged 65-74 years and <65 years.
CONCLUSION:
Hypogonadal men ≥65 years old showed significant benefit from TRT over 12 months, similar to that found for hypogonadal men <65 years old. TRT was well tolerated in older patients, successfully increased testosterone level regardless of age, and did not significantly increase PSA levels in older men.
Indian J Urol. 2012 Apr;28(2):123-8.
Testosterone replacement and prostate cancer.
Ramasamy R, Fisher ES, Schlegel PN.
Source
Department of Urology, New York - Presbyterian Hospital, Weill Cornell Medical College, New York, USA.
Abstract
This article is intended as a review of the available clinical data outlining the risks and benefits of testosterone (androgen) replacement therapy, specifically addressing the issue of the relationship between exogenous androgen administration and prostate cancer risk. There is controversy over whether androgen replacement is a risk factor for incident prostate cancer. Our review of current clinical information revealed that to date, no study or review has definitively shown that androgen replacement therapy is an independent risk factor for development of prostate cancer. Androgen administration seems to be beneficial in decreasing fatal cardiovascular events, body fat mass, and insulin resistance. Overall, the current clinical data seems to suggest that androgen replacement is an appropriate therapeutic option for men with symptomatic hypogonadism provided that patients continue to receive regular prostate screenings.
Actas Urol Esp. 2012 Jul 19. [Epub ahead of print]
Prevalence of Co-Morbidities in Patients With Erectile Dysfunction.
Martínez-Jabaloyas JM.
Source
Servicio de Urología, Hospital Clínico Universitario, Valencia, España.
Abstract
INTRODUCTION:
Erectile dysfunction (ED) is a multifactorial process which requires an integral approach. It is also a sentinel symptom of endothelial dysfunction that opens a door to the overall health of a man.
OBJECTIVES:
To analyze the prevalence of cardiovascular risk factors and other disorders in patients with ED. The relationship between the severity of ED and the total serum testosterone level and the therapeutic approach of doctors were also analyzed.
MATERIAL AND METHODS:
An observational, multicenter, national study in patients > 18 years who came to uroandrology or primary care consultations. Sociodemographic, anthropometric, lifestyle habits and medical history data of patients and the physician's therapeutic approach, were all collected. ED was diagnosed and total testosterone was assessed when necessary.
RESULTS:
1340 patients aged from 22-81 years took part in the study. Age was the most prevalent factor to develop the condition. Abdominal obesity, diabetes, and smoking had a high prevalence. Half of the patients presented psychological and/or sexual problems. 33% and 13.5% of patients had suboptimal levels of total testosterone (cut-off point of 12 nmol/l and 8 nmol/l, respectively), with a direct relationship with disease severity.
CONCLUSION:
Our study supports the need to examine cardiovascular risk factors in patients with ED and to identify patients who might benefit from testosterone replacement therapy. Psychological disorders should receive specialized care.
Below are a bunch of boring articles pasted directly from medical journals.
They are not so much for lay people to read and understand as just to convince you that I am not kidding about all of the stuff I said above about testosterone replacement.
J Clin Endocrinol Metab. 2012 Jun;97(6):2050-8. Epub 2012 Apr 11.
Testosterone treatment and mortality in men with low testosterone levels.
Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM.
Source
Veterans Affairs Puget Sound Health Care System, 1660 South Columbian Way, S-116PES, Seattle, Washington 98108, USA. [email protected]
Abstract
CONTEXT:
Low testosterone levels in men have been associated with increased mortality. However, the influence of testosterone treatment on mortality in men with low testosterone levels is not known.
OBJECTIVE:
The objective of the study was to examine the association between testosterone treatment and mortality in men with low testosterone levels.
DESIGN:
This was an observational study of mortality in testosterone-treated compared with untreated men, assessed with time-varying, adjusted Cox proportional hazards regression models. Effect modification by age, diabetes, and coronary heart disease was tested a priori.
SETTING:
The study was conducted with a clinical database that included seven Northwest Veterans Affairs medical centers.
PATIENTS:
Patients included a cohort of 1031 male veterans, aged older than 40 yr, with low total testosterone [≤250 ng/dl (8.7 nmol/liter)] and no history of prostate cancer, assessed between January 2001 and December 2002 and followed up through the end of 2005.
MAIN OUTCOME MEASURE:
Total mortality in testosterone-treated compared with untreated men was measured.
RESULTS:
Testosterone treatment was initiated in 398 men (39%) during routine clinical care. The mortality in testosterone-treated men was 10.3% compared with 20.7% in untreated men (P<0.0001) with a mortality rate of 3.4 deaths per 100 person-years for testosterone-treated men and 5.7 deaths per 100 person-years in men not treated with testosterone. After multivariable adjustment including age, body mass index, testosterone level, medical morbidity, diabetes, and coronary heart disease, testosterone treatment was associated with decreased risk of death (hazard ratio 0.61; 95% confidence interval 0.42-0.88; P = 0.008). No significant effect modification was found by age, diabetes, or coronary heart disease.
CONCLUSIONS:
In an observational cohort of men with low testosterone levels, testosterone treatment was associated with decreased mortality compared with no testosterone treatment. These results should be interpreted cautiously because residual confounding may still be a source of bias. Large, randomized clinical trials are needed to better characterize the health effects of testosterone treatment in older men with low testosterone levels.
J Urol. 2012 Apr;187(4):1369-73. Epub 2012 Feb 15.
Performance of total testosterone measurement to predict free testosterone for the biochemical evaluation of male hypogonadism.
Anawalt BD, Hotaling JM, Walsh TJ, Matsumoto AM.
Source
Department of Medicine, University of Washington and Geriatric Research, Seattle, Washington 98195, USA. [email protected]
Abstract
PURPOSE:
Guidelines recommend serum total testosterone measurement as the initial test to evaluate male hypogonadism, reserving free testosterone assessment for men with suspected sex hormone-binding globulin abnormalities or total testosterone near the lower limit of normal. We determined the performance of total testosterone measurement as a test to identify men with normal vs low free testosterone.
MATERIALS AND METHODS:
We examined the electronic medical records of all 3,672 men evaluated for hypogonadism by a serum testosterone panel, including total testosterone, sex hormone-binding globulin, albumin and calculated free testosterone, from January 1, 1997 through December 31, 2007 in a network that serves veterans in Washington.
RESULTS:
The sensitivity and specificity of low total testosterone (less than 280 ng/dl) to rule out and predict low calculated free testosterone was 91.0% and 73.7%, respectively. At thresholds of less than 350 and less than 400 ng/dl the sensitivity of total testosterone for low calculated free testosterone increased to 96.8% and 98.2%, and at thresholds of less than 150 and less than 200 ng/dl specificity increased to 98.9% and 92.6%, respectively.
CONCLUSIONS:
Total testosterone between 280 and 350 ng/dl is not sensitive enough to reliably exclude hypogonadism. Total testosterone must exceed 350 to 400 ng/dl to reliably predict normal free testosterone. Except when levels are less than 150 ng/dl total testosterone measurement has low specificity for the biochemical diagnosis of hypogonadism.
J Clin Endocrinol Metab. 2012 Aug;97(8):2809-17. Epub 2012 Jun 1.
Impact of male hormonal contraception on prostate androgens and androgen action in healthy men: a randomized, controlled trial.
Mostaghel EA, Lin DW, Amory JK, Wright JL, Marck BT, Nelson PS, Matsumoto AM, Bremner WJ, Page ST.
Source
AssociateDivision of Metabolism, Endocrinology, and Nutrition, University of Washington School of Medicine, Box 357138, 1959 NE Pacific Street, Seattle, Washington 98195. [email protected].
Abstract
Context: Male hormonal contraception (MHC) combines hypothalamic-pituitary-gonadal axis blockade with exogenous androgen delivery to maintain extragonadal androgen end-organ effects. Concern exists that MHC may adversely impact prostate health. Objective: The objective of the study was to determine the molecular impact of MHC on intraprostatic androgen concentrations and androgen action. Design: This was a single-blind, randomized, placebo-controlled study. Setting: The study was conducted at an academic medical center. Participants: 32 healthy men aged 25-55 yr participated in the study. Intervention: Interventions included placebo, daily transdermal testosterone (T) (T-gel), T-gel + depomedroxyprogesterone acetate (T+DMPA), or T-gel + dutasteride daily (T+D) for 12 wk, and prostate biopsy during treatment wk 10. Main Outcome Measures: Serum and prostate androgen concentrations and prostate epithelial-cell gene expression were measured. Results: Thirty men completed the study. Serum T levels were significantly increased in T-gel and T+D groups compared with baseline (P < 0.05) but were decreased with the addition of DMPA. Intraprostatic androgens were no different from placebo with T-gel treatment. Addition of DMPA to T resulted in 40% lower intraprostatic dihydrotestosterone (DHT) concentration (P = 0.0273 vs. placebo), whereas combining dutasteride with T resulted in a 90% decrease in intraprostatic DHT (P = 0.0012), 11-fold increased intraprostatic T (P = 0.0011), and 7-fold increased intraprostatic androstenedione (P = 0.0011). Significant differences in global or androgen-regulated prostate epithelial-cell gene expression were not observed. Androgen-regulated gene expression correlated with epithelial-cell androgen receptor and prostatic DHT in placebo, T-gel, and T+DMPA arms and with T and androstenedione levels in the T+D arm. Conclusions: MHC regimens do not markedly alter gene expression in benign prostate epithelium, suggesting they may not alter risk of prostate disease. Longer-term studies examining the impact of MHC on prostate health are needed.
J Urol. 2011 Feb;185(2):626-32. Epub 2010 Dec 18.
Oral testosterone with and without concomitant inhibition of 5α-reductase by dutasteride in hypogonadal men for 28 days.
Amory JK, Bush MA, Zhi H, Caricofe RB, Matsumoto AM, Swerdloff RS, Wang C, Clark RV.
Source
University of Washington, Seattle, Washington, USA.
Abstract
PURPOSE:
Co-administration of the 5α-reductase inhibitor dutasteride increases the oral testosterone bioavailability in men with experimentally induced hypogonadism. We examined oral testosterone with and without dutasteride administration in hypogonadal men for 28 days.
MATERIALS AND METHODS:
We randomly assigned 43 hypogonadal men to twice daily oral doses of 150, 250 or 400 mg testosterone with 0.25 mg dutasteride, 400 mg testosterone alone or 0.25 mg dutasteride alone for 28 days in a multicenter study. Subjects underwent pharmacokinetic profiling of serum hormones on days 1 and 28. A total of 32 men completed all study procedures.
RESULTS:
Serum testosterone increased in all groups on testosterone compared with that in the dutasteride only group. At the 400 mg dose the combination of testosterone and dutasteride resulted in average testosterone concentrations that were 2.7 and 4.6 times higher than in the testosterone only group on days 1 and 28, respectively (p <0.01). On day 28 average testosterone was 20% to 30% lower in all groups on testosterone and dutasteride, and 50% lower in the testosterone only group compared with day 1. Serum dihydrotestosterone was suppressed in all groups on dutasteride and increased in the testosterone only group.
CONCLUSIONS:
Oral testosterone administration resulted in a therapeutic serum testosterone concentration in hypogonadal men. Dutasteride improved the oral bioavailability of testosterone while suppressing dihydrotestosterone. Compared with day 1, testosterone was decreased after 28 days of administration. Additional study is warranted of oral testosterone with dutasteride for testosterone deficiency.
J Clin Endocrinol Metab. 2010 Jun;95(6):2536-59.
Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline.
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, Montori VM; Task Force, Endocrine Society.
Source
Boston University School of Medicine, Boston, Massachusetts 02118, USA.
Abstract
OBJECTIVE:
Our objective was to update the guidelines for the evaluation and treatment of androgen deficiency syndromes in adult men published previously in 2006.
PARTICIPANTS:
The Task Force was composed of a chair, selected by the Clinical Guidelines Subcommittee of The Endocrine Society, five additional experts, a methodologist, and a medical writer. The Task Force received no corporate funding or remuneration.
CONCLUSIONS:
We recommend making a diagnosis of androgen deficiency only in men with consistent symptoms and signs and unequivocally low serum testosterone levels. We suggest the measurement of morning total testosterone level by a reliable assay as the initial diagnostic test. We recommend confirmation of the diagnosis by repeating the measurement of morning total testosterone and, in some men in whom total testosterone is near the lower limit of normal or in whom SHBG abnormality is suspected by measurement of free or bioavailable testosterone level, using validated assays. We recommend testosterone therapy for men with symptomatic androgen deficiency to induce and maintain secondary sex characteristics and to improve their sexual function, sense of well-being, muscle mass and strength, and bone mineral density. We recommend against starting testosterone therapy in patients with breast or prostate cancer, a palpable prostate nodule or induration or prostate-specific antigen greater than 4 ng/ml or greater than 3 ng/ml in men at high risk for prostate cancer such as African-Americans or men with first-degree relatives with prostate cancer without further urological evaluation, hematocrit greater than 50%, untreated severe obstructive sleep apnea, severe lower urinary tract symptoms with International Prostate Symptom Score above 19, or uncontrolled or poorly controlled heart failure. When testosterone therapy is instituted, we suggest aiming at achieving testosterone levels during treatment in the mid-normal range with any of the approved formulations, chosen on the basis of the patient's preference, consideration of pharmacokinetics, treatment burden, and cost. Men receiving testosterone therapy should be monitored using a standardized plan.
Endocr J. 2012 Aug 31. [Epub ahead of print]
Increased frequency of anxiety, depression, quality of life and sexual life in young hypogonadotropic hypogonadal males and impacts of testosterone replacement therapy on these conditions.
Aydogan U, Aydogdu A, Akbulut H, Sonmez A, Yuksel S, Basaran Y, Uzun O, Bolu E, Saglam K.
Source
Department of Family Medicine, Gulhane School of Medicine, Ankara 06018, Turkey.
Abstract
Hypogonadotropic hypogonadism is defined as the failure in production of gonadal hormones, thus resulting in lower amounts of testosterone. Depression, anxiety and decreased quality of life are the most common psychopathological conditions in young hypogonadal men. The aim of the present study was to assess the still debated relationship with testosterone levels and psychological symptoms in young male patients with congenital hypogonadotropic hypogonadism (CHH). 39 young male patients with CHH and 40 age-matched healthy males were enrolled in the present study. The impact of testosterone replacement treatment (TRT) on the patients' anxiety and depression levels, sexual function and quality of life were assessed before and after 6 months of treatment using valid and reliable scales, including the Short Form-36 (SF-36), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Arizona Sexual Experiences (ASEX). Patients with CHH had significantly higher scores for BDI, BAI, and ASEX than the control subjects at baseline (p=0.011, p=0.036, p<0.001, respectively). The ASEX and BDI scores significantly improved after the TRT (p<0.001 for both), while the improvement in the BAI score was not statistically significant (p=0.135). When compared to the control group, treatment naïve hypogonadal patients had more severe symptoms of sexual dysfunction, anxiety, depression, and worse quality of life. After 6 months of TRT, we observed improvements in the above parameters, suggesting that low endogenous levels of testosterone might be related to the increased incidence of psychological symptoms.
Metabolism. 2012 Sep 19. pii: S0026-0495(12)00316-2. doi: 10.1016/j.metabol.2012.08.012. [Epub ahead of print]
The complex interaction between obesity, metabolic syndrome and reproductive axis: A narrative review.
Michalakis K, Mintziori G, Kaprara A, Tarlatzis BC, Goulis DG.
Source
First Department of Internal Medicine, Laikon University Hospital, Athens University Medical School, Greece.
Abstract
The aim of this narrative review is to provide current evidence for the interaction between obesity, metabolic syndrome (MS) and reproductive axis. Gonadotropin-releasing hormone (GnRH) pulses and, consequently, normal function of reproductive (hypothalamus-pituitary-gonadal) axis depend on normal energy balance, which presupposes sufficient food intake, reasonable energy consumption and average thermoregulatory costs. In case of an energy imbalance, reproductive dysfunction may occur. In young women, excessive leanness is accompanied by puberty delay, whereas premature puberty might be a manifestation of obesity. In a similar way, obesity in men affects fertility. Excess adipose tissue results in increased conversion of testosterone to estradiol, which may lead to secondary hypogonadism through reproductive axis suppression. Moreover, oxidative stress at the level of the testicular micro-environment may result in decreased spermatogenesis and sperm damage. Products of the adipocyte, such as leptin, adiponectin and resistin, and gut peptides, such as ghrelin, are considered to be crucial in the interaction between energy balance and reproduction. Finally, an indirect evidence for the interplay between MS and reproductive axis is the fact that when treating components of one, parameters of the other can be improved as well. These therapeutic interventions include lifestyle modifications, pharmacological agents, such as sex hormonereplacement therapy, and surgical procedures. Although many issues remain unclear, the elucidation of the complex interaction between MS and reproductive axis will have obvious clinical implications in the therapeutic approach of both entities.
Int J Impot Res. 2012 Sep 13. doi: 10.1038/ijir.2012.29. [Epub ahead of print]
Testosterone replacement therapy in the setting of prostate cancer treated with radiation.
Pastuszak AW, Pearlman AM, Godoy G, Miles BJ, Lipshultz LI, Khera M.
Source
Scott Department of Urology, Baylor College of Medicine, Houston, TX, USA.
Abstract
A lack of consensus and few data support testosterone replacement therapy (TRT) in hypogonadal men who have been treated for prostate cancer (CaP), particularly those who have received radiation therapy. We performed retrospective review of 13 hypogonadal men with CaP, treated with brachytherapy or external beam radiotherapy who were subsequently treated with testosterone (T) between 2006 and 2011. Serum T, free T (FT), estrogen (E), sex hormone-binding globulin (SHBG), prostate-specific antigen (PSA), hemoglobin (Hgb) and hematocrit (Hct) values were evaluated approximately every 3 months after TRT initiation up to 67 months of follow-up. Prostate biopsies demonstrated four men with Gleason (Gl) 6, 7 with Gl 7 and 2 with Gl 8 disease. Median (interquartile range) age at TRT initiation was 68.0 (62.0-77.0) years, initial T 178.0 (88.0-263.5) ng dl(-1), FT 10.1 (5.7-15.0) pg ml(-1) and PSA 0.30 (0.06-0.95) ng ml(-1). Median follow-up after TRT initiation was 29.7 months (range 2.3-67.3 months). At median follow-up, a significant increase in mean T (368.0 (281.3-591.0) ng dl(-1), P=0.012) and SHBG were observed, with no significant increases in Hgb, Hct, E, FT, or PSA (0.66 (0.16-1.35) ng ml(-1), P=0.345). No significant increases in PSA or CaP recurrences were observed at any follow-up interval. TRT in the setting of CaP after treatment with radiation therapy results in a rise in serum T levels and improvement in hypogonadal symptoms without evidence of CaP recurrence or progression.International Journal of Impotence Research advance online publication, 13 September 2012; doi:10.1038/ijir.2012.29.
Clin Interv Aging. 2012;7:321-30. Epub 2012 Aug 24.
Testosterone replacement therapy among elderly males: the Testim Registry in the US (TRiUS).
Bhattacharya RK, Khera M, Blick G, Kushner H, Miner MM.
Source
Department of Internal Medicine, University of Kansas Medical Center, Kansas City, KS, USA;
Abstract
BACKGROUND:
Testosterone levels naturally decline with age in men, often resulting in testosterone deficiency (hypogonadism). However, few studies have examined hypogonadal characteristics and treatment in older (≥65 years) men.
OBJECTIVE:
To compare data at baseline and after 12 months of testosterone replacement therapy (TRT) in hypogonadal men ≥65 vs <65 years old. Data for participants 65-74 vs ≥75 years old were also compared.
METHODS:
Data were from TRiUS (Testim Registry in the United States), which enrolled 849 hypogonadal men treated with Testim(®) 1% (50-100 mg testosterone gel/day) for the first time. Anthropometric, laboratory, and clinical measures were taken at baseline and 12 months, including primary outcomes of total testosterone (TT), free testosterone (FT), and prostate-specific antigen (PSA) levels. Comparisons of parameters were made using Fisher's exact test or analysis of variance. Nonparametric Spearman's ρ and first-order partial correlation coefficients adjusted for the effect of age were used to examine bivariate correlations among parameters.
RESULTS:
Of the registry participants at baseline with available age information, 16% (133/845) were ≥65 years old. They were similar to men <65 years old in the duration of hypogonad-ism prior to enrollment (∼1 year), TT and FT levels at baseline, TT and FT levels at 12-month follow-up, and in reported compliance with treatment. Older patients were more likely to receive lower doses of TRT. PSA levels did not statistically differ between groups after 12 months of TRT (2.18 ± 2.18 ng/mL for ≥65 vs 1.14 ± 0.84 ng/mL for <65 years old, P = 0.1). Baseline values for the >75-year-old subcohort were not significantly different from subcohorts aged 65-74 years and <65 years.
CONCLUSION:
Hypogonadal men ≥65 years old showed significant benefit from TRT over 12 months, similar to that found for hypogonadal men <65 years old. TRT was well tolerated in older patients, successfully increased testosterone level regardless of age, and did not significantly increase PSA levels in older men.
Indian J Urol. 2012 Apr;28(2):123-8.
Testosterone replacement and prostate cancer.
Ramasamy R, Fisher ES, Schlegel PN.
Source
Department of Urology, New York - Presbyterian Hospital, Weill Cornell Medical College, New York, USA.
Abstract
This article is intended as a review of the available clinical data outlining the risks and benefits of testosterone (androgen) replacement therapy, specifically addressing the issue of the relationship between exogenous androgen administration and prostate cancer risk. There is controversy over whether androgen replacement is a risk factor for incident prostate cancer. Our review of current clinical information revealed that to date, no study or review has definitively shown that androgen replacement therapy is an independent risk factor for development of prostate cancer. Androgen administration seems to be beneficial in decreasing fatal cardiovascular events, body fat mass, and insulin resistance. Overall, the current clinical data seems to suggest that androgen replacement is an appropriate therapeutic option for men with symptomatic hypogonadism provided that patients continue to receive regular prostate screenings.
Actas Urol Esp. 2012 Jul 19. [Epub ahead of print]
Prevalence of Co-Morbidities in Patients With Erectile Dysfunction.
Martínez-Jabaloyas JM.
Source
Servicio de Urología, Hospital Clínico Universitario, Valencia, España.
Abstract
INTRODUCTION:
Erectile dysfunction (ED) is a multifactorial process which requires an integral approach. It is also a sentinel symptom of endothelial dysfunction that opens a door to the overall health of a man.
OBJECTIVES:
To analyze the prevalence of cardiovascular risk factors and other disorders in patients with ED. The relationship between the severity of ED and the total serum testosterone level and the therapeutic approach of doctors were also analyzed.
MATERIAL AND METHODS:
An observational, multicenter, national study in patients > 18 years who came to uroandrology or primary care consultations. Sociodemographic, anthropometric, lifestyle habits and medical history data of patients and the physician's therapeutic approach, were all collected. ED was diagnosed and total testosterone was assessed when necessary.
RESULTS:
1340 patients aged from 22-81 years took part in the study. Age was the most prevalent factor to develop the condition. Abdominal obesity, diabetes, and smoking had a high prevalence. Half of the patients presented psychological and/or sexual problems. 33% and 13.5% of patients had suboptimal levels of total testosterone (cut-off point of 12 nmol/l and 8 nmol/l, respectively), with a direct relationship with disease severity.
CONCLUSION:
Our study supports the need to examine cardiovascular risk factors in patients with ED and to identify patients who might benefit from testosterone replacement therapy. Psychological disorders should receive specialized care.
Nov 2013 Testosterone replacement dangerous for men with heart disease. Maybe !
Testosterone gel controversy
Typical studies of testosterone effects have 5000 - 15,000 people in them. ( Mostly men, unless you are the JAMA ! ) It takes a lot of test subjects to be able to sort out the wierd outliers.
This study only had 135 people, so it doesn't have much of what is called "statistical power". But it is something to keep in mind, because - if correct - it could mean that testosterone gels ( and only the gels ) may increase coronary artery disease.Testosterone
Gel Speeds AtherosclerosisAnd finally, the use of topical testosterone could speed up atherosclerosis in older men. This was the major finding of an National Institutes of Health trial[1] that examined clinical outcomes in older men with age-related low testosterone levels.
The randomized trial involved 138 men with a mean age of 71 years who had subjective and objective evidence of sexual dysfunction, physical dysfunction, and/or reduced vitality. Many, like expected, had cardiovascular risk factors. Half of the men had severe atherosclerosis before starting testosterone treatment.
The plan was to achieve testosterone levels of men 40 years younger. The trial's hypothesis was that testosterone therapy would slow the progression of noncalcified coronary artery plaque volume.
But they found that men who used testosterone gel for a year had a 20% higher buildup of noncalcified plaque in their coronary arteries compared with those who used a placebo gel. The trial wasn't long enough to determine whether testosterone would also lead to an increase in cardiovascular events, but this information leads us to be cautious in prescribing testosterone to men with cardiovascular risk factors.
This study only had 135 people, so it doesn't have much of what is called "statistical power". But it is something to keep in mind, because - if correct - it could mean that testosterone gels ( and only the gels ) may increase coronary artery disease.Testosterone
Gel Speeds AtherosclerosisAnd finally, the use of topical testosterone could speed up atherosclerosis in older men. This was the major finding of an National Institutes of Health trial[1] that examined clinical outcomes in older men with age-related low testosterone levels.
The randomized trial involved 138 men with a mean age of 71 years who had subjective and objective evidence of sexual dysfunction, physical dysfunction, and/or reduced vitality. Many, like expected, had cardiovascular risk factors. Half of the men had severe atherosclerosis before starting testosterone treatment.
The plan was to achieve testosterone levels of men 40 years younger. The trial's hypothesis was that testosterone therapy would slow the progression of noncalcified coronary artery plaque volume.
But they found that men who used testosterone gel for a year had a 20% higher buildup of noncalcified plaque in their coronary arteries compared with those who used a placebo gel. The trial wasn't long enough to determine whether testosterone would also lead to an increase in cardiovascular events, but this information leads us to be cautious in prescribing testosterone to men with cardiovascular risk factors.