I have a prostate ...
I am pretty sure I have one.
I haven't seen it lately, but I am sure it is hiding there behind me somewhere. Someone may have put their finger on it recently.
And I wonder constantly if it is going to get me into trouble. And if it does, what I am going to do about it ? I actually have no idea what I would do. Which is a bit of a problem, because I am sort of a prostate person.
There are two basic things that can go wrong with a prostate.
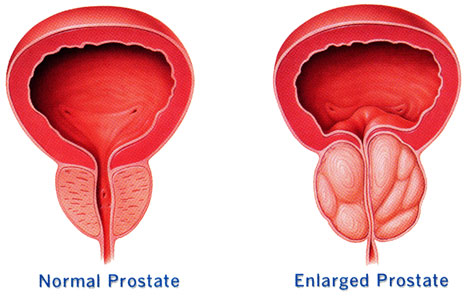
a) (Benign Prostatic Hypertrophy) , which happens to all of us as we get older. This just means the prostate gets bigger and we get older. And it happens to everyone.
b) (Prostate Cancer) . Which also happens to all of us as we get older too.
But prostate cancer is a slow growing and secretive type of tumor. There is a huge difference between dying with prostate cancer and dying of prostate cancer.
So no one is quite sure of the best way to diagnose prostate cancer. And once it is diagnosed, no one is sure what the best treatment is - or if the best treatment is no treatment at all.
And hence our little saga begins ....
I haven't seen it lately, but I am sure it is hiding there behind me somewhere. Someone may have put their finger on it recently.
And I wonder constantly if it is going to get me into trouble. And if it does, what I am going to do about it ? I actually have no idea what I would do. Which is a bit of a problem, because I am sort of a prostate person.
There are two basic things that can go wrong with a prostate.
a) (Benign Prostatic Hypertrophy) , which happens to all of us as we get older. This just means the prostate gets bigger and we get older. And it happens to everyone.
b) (Prostate Cancer) . Which also happens to all of us as we get older too.
But prostate cancer is a slow growing and secretive type of tumor. There is a huge difference between dying with prostate cancer and dying of prostate cancer.
So no one is quite sure of the best way to diagnose prostate cancer. And once it is diagnosed, no one is sure what the best treatment is - or if the best treatment is no treatment at all.
And hence our little saga begins ....
Overview of Prostate Propaganda
Prostate Cancer(Prostate Problems, Cancer of the Prostate)
In this factsheet:
Facts:
- Prostate cancer is the most often diagnosed cancer in Canadian men, aside from skin cancers
- ranks third as a cause of cancer death in Canadian men aged 65 and over.
- the average male has a 0.05% chance of dying of prostate cancer. - the means that the average male has a 99.5% chance of dying from something other than prostate cancer
-prostate cancer is a slow growing indolent disease with 99% 5 year survival after diagnosis
- by the age of 50, about 30-50% of men will harbour a small insignificant focus of prostate cancer
- the prostate produces the liquid that moves sperm.
- is a walnut shaped gland between the rectum and the pubic bone, beneath the bladder
Causes of Prostate Cancer
- some people are predisposed by a genetic mutation. This means if you have family members affected you are at increased risk.
- risk is twice as high in men of African descent ( ie black guys )
Risk Factors
Some foods may protect against prostate cancer.
- Tomatoes, grapefruit, and watermelon all contain lycopene, a chemical that may lower risk of prostate cancer.
- vitamins E, selenium, and cruciferous vegetables like broccoli, cauliflower, Brussels sprouts, and bok choy may be mildly protective.
- high doses of zinc supplements (more than 100 mg daily) may lead to an increased risk of developing the condition.
Symptoms:
- most cancers are small and cause no symptoms
- that is why they are only discovered during blood screening tests or surgery for benign prostatic hyperplasia, which often does cause noticeable symptoms.
Large, tumours can press on other organs such as the bladder, causing incontinence (reduced bladder control) or making urination difficult or painful, or causing erectile dysfunction ( by pressure on the nerves leading to the penis. )
Advanced tumours can also cause:
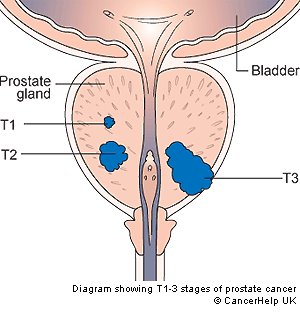
Risk stratification and staging
People with localized (non-metastatic) prostate cancer may be characterized as low-, intermediate-, or high-risk for prostate cancer mortality. PSA level is one of three variables on which the risk-stratification is based; the others are the grade of prostate cancer (Gleason grading system) and the stage of cancer based on physical examination and imaging studies. Criteria for each risk category are as follows:
Low-risk: PSA < 10, Gleason score ≤ 6, AND clinical stage ≤ T2a
Intermediate-risk: PSA 10-20, Gleason score 7, OR clinical stage T2b/c
High-risk: PSA > 20, Gleason score ≥ 8, OR clinical stage ≥ T3
Researchers are working to identify more accurate prognostic variables for risk-stratification of prostate cancer.
Diagnosing and Treating Prostate Cancer
In this factsheet:
- The Facts on Prostate Cancer
- Causes of Prostate Cancer
- Symptoms and Complications of Prostate Cancer
- Diagnosing Prostate Cancer
- Treating and Preventing Prostate Cancer
Facts:
- Prostate cancer is the most often diagnosed cancer in Canadian men, aside from skin cancers
- ranks third as a cause of cancer death in Canadian men aged 65 and over.
- the average male has a 0.05% chance of dying of prostate cancer. - the means that the average male has a 99.5% chance of dying from something other than prostate cancer
-prostate cancer is a slow growing indolent disease with 99% 5 year survival after diagnosis
- by the age of 50, about 30-50% of men will harbour a small insignificant focus of prostate cancer
- the prostate produces the liquid that moves sperm.
- is a walnut shaped gland between the rectum and the pubic bone, beneath the bladder
Causes of Prostate Cancer
- some people are predisposed by a genetic mutation. This means if you have family members affected you are at increased risk.
- risk is twice as high in men of African descent ( ie black guys )
Risk Factors
- age: especially over 65
- family history: having a father or brother with prostate cancer doubles your risk
- Blacks have higher risk, Orientals have lower risk
- geography: prostate cancer is rarer in Asia, Africa, and South America
- weight, physical inactivity: overweight and inactive men have higher rates of prostate cancer
- diet: eating high-fat foods and red meats, and not eating enough vegetables, fruits, and fibre
- Research has shown a link between high saturated-fat diets and prostate cancer.
- Some experts argue that a lack of fruits and vegetables is the problem, and that people with high-fat diets get more cancer because they tend not to eat enough vegetables.
- very high calcium intake has also been linked to prostate cancer.
- balding, especially before the age of twenty, may be associated with increased risk
Some foods may protect against prostate cancer.
- Tomatoes, grapefruit, and watermelon all contain lycopene, a chemical that may lower risk of prostate cancer.
- vitamins E, selenium, and cruciferous vegetables like broccoli, cauliflower, Brussels sprouts, and bok choy may be mildly protective.
- high doses of zinc supplements (more than 100 mg daily) may lead to an increased risk of developing the condition.
Symptoms:
- most cancers are small and cause no symptoms
- that is why they are only discovered during blood screening tests or surgery for benign prostatic hyperplasia, which often does cause noticeable symptoms.
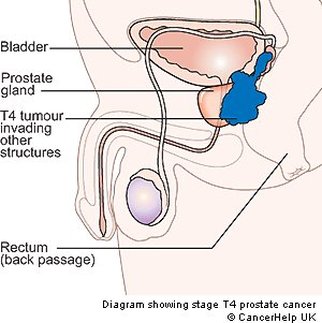
Large, tumours can press on other organs such as the bladder, causing incontinence (reduced bladder control) or making urination difficult or painful, or causing erectile dysfunction ( by pressure on the nerves leading to the penis. )
Advanced tumours can also cause:
- pain by pressing on the spine or pelvis
- burning or pain when urinating
- frequent urination
- pain when ejaculating
- blood to appear in the urine or semen
- pain or stiffness in the lower back, hips, or upper thighs
- The lymphatic system is the main carrier of metastases in prostate cancer. Secondary tumours can grow almost anywhere in the body, such as the lungs, brain, lymph nodes, however, it is most likely to spread to the bone.
Risk stratification and staging
People with localized (non-metastatic) prostate cancer may be characterized as low-, intermediate-, or high-risk for prostate cancer mortality. PSA level is one of three variables on which the risk-stratification is based; the others are the grade of prostate cancer (Gleason grading system) and the stage of cancer based on physical examination and imaging studies. Criteria for each risk category are as follows:
Low-risk: PSA < 10, Gleason score ≤ 6, AND clinical stage ≤ T2a
Intermediate-risk: PSA 10-20, Gleason score 7, OR clinical stage T2b/c
High-risk: PSA > 20, Gleason score ≥ 8, OR clinical stage ≥ T3
Researchers are working to identify more accurate prognostic variables for risk-stratification of prostate cancer.
Diagnosing and Treating Prostate Cancer
Diagnosing Prostate Cancer
Facts on Prostate Cancer
Causes of Prostate Cancer
Symptoms and Complications of Prostate Cancer
Diagnosing Prostate Cancer
Treating and Preventing Prostate Cancer
There is a screening test for prostate cancer called the prostate-specific antigen (PSA) test. PSA is made by prostate cells and all men have PSA levels that can be detected in the blood. Men with prostate cancer often have more PSA. High PSA levels can also occur with noncancerous conditions, and PSA may be low in people with prostate cancer. Therefore, repeat testing may be done to confirm the results. If high PSA levels are found repeatedly, doctors may suggest taking a biopsy. As people age, PSA test may become less reliable in identifying prostate cancer. You should discuss with your doctor about whether you require PSA testing.
Another test a doctor can do is a digital rectal exam(DRE), which involves feeling the prostate with a gloved finger. If there is a high PSA level, or a lump is felt, small tissue samples will be taken from about 10 to 12 locations in the prostate with the use of abiopsy gun. The doctor guides the biopsy gun with the aid of a transrectal ultrasound(TRUS), a device that creates an image of the prostate. The doctor will also want a biopsy sample of the lymph nodes to check if the disease has spread. You may have short periods of sharp pain during this procedure. Sometimes, doctors will freeze the area to help reduce the pain.
If cancer is found, a specialist (usually a urologist) will determine the size, stage, and grade of the tumour. This information will help determine which therapy may be used to treat the cancer.
Causes of Prostate Cancer
Symptoms and Complications of Prostate Cancer
Diagnosing Prostate Cancer
Treating and Preventing Prostate Cancer
There is a screening test for prostate cancer called the prostate-specific antigen (PSA) test. PSA is made by prostate cells and all men have PSA levels that can be detected in the blood. Men with prostate cancer often have more PSA. High PSA levels can also occur with noncancerous conditions, and PSA may be low in people with prostate cancer. Therefore, repeat testing may be done to confirm the results. If high PSA levels are found repeatedly, doctors may suggest taking a biopsy. As people age, PSA test may become less reliable in identifying prostate cancer. You should discuss with your doctor about whether you require PSA testing.
Another test a doctor can do is a digital rectal exam(DRE), which involves feeling the prostate with a gloved finger. If there is a high PSA level, or a lump is felt, small tissue samples will be taken from about 10 to 12 locations in the prostate with the use of abiopsy gun. The doctor guides the biopsy gun with the aid of a transrectal ultrasound(TRUS), a device that creates an image of the prostate. The doctor will also want a biopsy sample of the lymph nodes to check if the disease has spread. You may have short periods of sharp pain during this procedure. Sometimes, doctors will freeze the area to help reduce the pain.
If cancer is found, a specialist (usually a urologist) will determine the size, stage, and grade of the tumour. This information will help determine which therapy may be used to treat the cancer.
Preventing and Treating Prostate Cancer !

Prostate tumours grow slowly, often over a period of 10 years or more and are non-aggressive compared to most other types of cancer. They also tend to appear late in life. Especially in older men, small tumours are often left in place without any treatment. However, the doctor will check regularly to be sure the cancer isn't growing faster than expected. If this occurs, treatment will be started. The doctor will follow the cancer closely to make sure that treatment is started early enough so that it is still possible to remove all of the cancer. This is known as "active surveillance."
Cancer that has spread far beyond the prostate requires a range of antitumour and pain-killing treatments.
Cancer that hasn't spread beyond the prostate is usually treated with surgery or radiation.
a) Radiation Therapy - often the first choice for Prostate Ca therapy
Your doctor may use either an external beam, or occasionally radioactive seed implants inserted into or near the prostate through surgery (called brachytherapy) to destroy cancer cells. Researchers are looking for new ways to deliver radiation therapy, as well as the potential use of hormone therapy at the same time as radiation therapy (see the information below about hormone therapy).
b) Surgery
, the standard operation is radical prostatectomy, the complete removal of the prostate gland. An incision is made either in the lower abdomen or between the anus and scrotum, and the prostate gland is removed. This is the method most likely to cure prostate cancer.
Removal of the prostate can have major side effects, including impotence and incontinence. A man's ability to have an erection after surgery depends on whether the nerves next to the prostate have been damaged. Sometimes, the nerves are affected by cancer and must be removed. Other times, the doctor tries to leave them in place but impotence occurs anyway. Your doctor should be consulted about the likelihood of a "nerve-sparing" procedure in any specific case.
When deciding on whether surgery or radiation is the best choice to treat prostate cancer, both the doctor and patient need to discuss the risks and benefits. Both forms of treatment have complications, such as bladder irritation, sexual dysfunction, and bowel symptoms, and the decision will depend upon the disease extent, general health, and preferences of the individual patient.
Sometimes the cancerous tissue is killed with a cold probe (cryosurgery) that freezes it. This technique can also cause impotence. It's fairly new, so we don't know if long-term results are as good as those of radical prostatectomy.
c) Hormonal Therapy
involves reducing the levels of the hormones like testosterone (called androgens) or blocking the cancer cells from detecting those hormones. Prostate cancer cells rely on androgens to grow. This treatment can also cause the prostate to shrink. It won't cure the cancer, but it can control the growth of the tumour and may be useful before surgery, especially cryosurgery. Instead of using medications, some men may choose to reduce their levels of testosterone by having their testicles removed (orchiectomy).
Both hormones and radiation are common treatments in patients whose cancer has spread or come back after surgery. Normal cancer chemotherapy is not commonly used for prostate cancer, except to relieve symptoms caused by metastases.
Your doctor will discuss treatment options based on the size, type, and location of the cancer.
If you are worried about developing prostate cancer, you should ask your doctor about PSA testing and digital rectal exams
Cancer that has spread far beyond the prostate requires a range of antitumour and pain-killing treatments.
Cancer that hasn't spread beyond the prostate is usually treated with surgery or radiation.
a) Radiation Therapy - often the first choice for Prostate Ca therapy
Your doctor may use either an external beam, or occasionally radioactive seed implants inserted into or near the prostate through surgery (called brachytherapy) to destroy cancer cells. Researchers are looking for new ways to deliver radiation therapy, as well as the potential use of hormone therapy at the same time as radiation therapy (see the information below about hormone therapy).
b) Surgery
, the standard operation is radical prostatectomy, the complete removal of the prostate gland. An incision is made either in the lower abdomen or between the anus and scrotum, and the prostate gland is removed. This is the method most likely to cure prostate cancer.
Removal of the prostate can have major side effects, including impotence and incontinence. A man's ability to have an erection after surgery depends on whether the nerves next to the prostate have been damaged. Sometimes, the nerves are affected by cancer and must be removed. Other times, the doctor tries to leave them in place but impotence occurs anyway. Your doctor should be consulted about the likelihood of a "nerve-sparing" procedure in any specific case.
When deciding on whether surgery or radiation is the best choice to treat prostate cancer, both the doctor and patient need to discuss the risks and benefits. Both forms of treatment have complications, such as bladder irritation, sexual dysfunction, and bowel symptoms, and the decision will depend upon the disease extent, general health, and preferences of the individual patient.
Sometimes the cancerous tissue is killed with a cold probe (cryosurgery) that freezes it. This technique can also cause impotence. It's fairly new, so we don't know if long-term results are as good as those of radical prostatectomy.
c) Hormonal Therapy
involves reducing the levels of the hormones like testosterone (called androgens) or blocking the cancer cells from detecting those hormones. Prostate cancer cells rely on androgens to grow. This treatment can also cause the prostate to shrink. It won't cure the cancer, but it can control the growth of the tumour and may be useful before surgery, especially cryosurgery. Instead of using medications, some men may choose to reduce their levels of testosterone by having their testicles removed (orchiectomy).
Both hormones and radiation are common treatments in patients whose cancer has spread or come back after surgery. Normal cancer chemotherapy is not commonly used for prostate cancer, except to relieve symptoms caused by metastases.
Your doctor will discuss treatment options based on the size, type, and location of the cancer.
If you are worried about developing prostate cancer, you should ask your doctor about PSA testing and digital rectal exams
Famous Men with Prostate Cancer
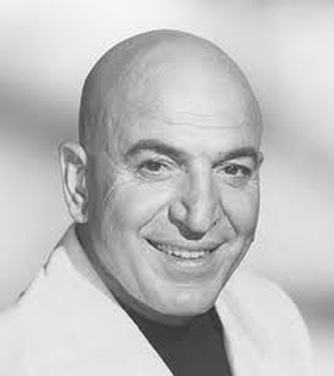
Telly Savalas - died of prostate ca at 70
The stereotypical risk person for prostate cancer would be a fat, bald, sedentary male who eats a hi fat diet and gets almost no exercise. In other words, Winston Churchill, and Kojak !
I don't know what actually did in Winny, but Telly Savalas actually did die of Prostate Cancer in 1994, at the age of 70.
Harry Belafonte - diagnosed in 1996, and successfully treated. Now a prostate Ca advocate.
Robert De Niro - diagnosed in 2003, at the age of 60. His father died of Prostate Ca at 71
Rudy Giuliani - former New York City mayor, was diagnosed in April 2000. Had radioactive seeds implanted in Sept 2000. Giuliani's father died of prostate Ca in 1981 at the age of 73.
Robert Goulet. Diagnosed in 1993 at age 60, following routine blood work for an insurance medical. Had a radical prostatectomy, and is now an advocate for prostate cancer.
Nelson Mandela - diagnosed on 2001, and is doing well post treatment.
Roger Moore - the former 007 was successfully treated with surgery in 1993.
Phil Lesh : The Grateful Dead bassist announced that he was diagnosed with early-stage prostate cancer in October 2006.
Timothy Leary: The 1960s counterculture icon died from the disease in 1996 at the age of 75.
Laurence Olivier: Diagnosed in 1967 and underwent radiation treatment that successfully eradicated the cancer.
Jerry Orbach: The Law and Order star died from the disease in Dec. 28, 2004 at the age of 69.
Linus Pauling: The Nobel Prize winner was diagnosed in 1991 at the age of 90 and died of the disease in 1994.
Colin Powell: In 2003, he underwent surgery for early-stage prostate cancer and made a full recovery.
Johnny Ramone: The Ramones guitarist died in 2004 at the age of 55 after a five-year battle with the disease.
Gen. H. Norman Schwarzkopf: Diagnosed in 1993 and underwent successful surgery.
Pierre Elliot Trudeau: The Prime Minister of Canada died of prostate cancer in 2000 at the age of 80.
Bishop Desmond Tutu: Diagnosed after a routine exam in 1996. He was treated in the United States with hormone therapy and radiation.
Earl Woods: Tiger Woods' father was diagnosed in 1998 and successfully treated with radiation, but the cancer returned more aggressively in 2004. Woods died on May 3, 2006 at the age of 74.
Frank Zappa: Died of complications from the disease on December 4, 1993 at the age of 52.
I don't know what actually did in Winny, but Telly Savalas actually did die of Prostate Cancer in 1994, at the age of 70.
Harry Belafonte - diagnosed in 1996, and successfully treated. Now a prostate Ca advocate.
Robert De Niro - diagnosed in 2003, at the age of 60. His father died of Prostate Ca at 71
Rudy Giuliani - former New York City mayor, was diagnosed in April 2000. Had radioactive seeds implanted in Sept 2000. Giuliani's father died of prostate Ca in 1981 at the age of 73.
Robert Goulet. Diagnosed in 1993 at age 60, following routine blood work for an insurance medical. Had a radical prostatectomy, and is now an advocate for prostate cancer.
Nelson Mandela - diagnosed on 2001, and is doing well post treatment.
Roger Moore - the former 007 was successfully treated with surgery in 1993.
Phil Lesh : The Grateful Dead bassist announced that he was diagnosed with early-stage prostate cancer in October 2006.
Timothy Leary: The 1960s counterculture icon died from the disease in 1996 at the age of 75.
Laurence Olivier: Diagnosed in 1967 and underwent radiation treatment that successfully eradicated the cancer.
Jerry Orbach: The Law and Order star died from the disease in Dec. 28, 2004 at the age of 69.
Linus Pauling: The Nobel Prize winner was diagnosed in 1991 at the age of 90 and died of the disease in 1994.
Colin Powell: In 2003, he underwent surgery for early-stage prostate cancer and made a full recovery.
Johnny Ramone: The Ramones guitarist died in 2004 at the age of 55 after a five-year battle with the disease.
Gen. H. Norman Schwarzkopf: Diagnosed in 1993 and underwent successful surgery.
Pierre Elliot Trudeau: The Prime Minister of Canada died of prostate cancer in 2000 at the age of 80.
Bishop Desmond Tutu: Diagnosed after a routine exam in 1996. He was treated in the United States with hormone therapy and radiation.
Earl Woods: Tiger Woods' father was diagnosed in 1998 and successfully treated with radiation, but the cancer returned more aggressively in 2004. Woods died on May 3, 2006 at the age of 74.
Frank Zappa: Died of complications from the disease on December 4, 1993 at the age of 52.